-
Posts
587 -
Joined
-
Last visited
-
Days Won
32
Content Type
Profiles
Forums
Gallery
Downloads
Events
Store
Posts posted by David S. Kozin
-
-
HPPD STUDY IDEA:
Prepulse Inhibition Study and Event-related Oscillations from Evoked Potentials: (P300 EEG, EMG & ERP)
Mid-latency evoked responses are so designated to differentiate them from the earlier sensory potentials and later ERPs that
are more affected by cognitive processing. The ERP measures that appear most important are the three most examined midlatency components in the auditory modality that are designated P50 (a positive component occurring between 35 and 80 ms
after stimulus onset), N100 (a negative component occurring between 80 and 150 ms after stimulus onset), and P200 (a
positive component occurring between 150 and 250 ms after stimulus onset). These components share the characteristic that
their amplitude decreases with repetition (habituation or sensory gating).
The P50 and N100 components have been studied extensively in psychiatric patients. Sensory gating of P50 is a potentially
useful endophenotype of psychosis or latent psychosis. Evidence for an inhibitory abnormality (i.e., sensory gating deficit) in
schizophrenic patients has been around for almost 25 years. The magnitude of the deficit is similar to the most robust
findings reported in neuroimaging and neuropsychology in schizophrenia. The N100 electrode component has also been
recently shown to exhibit a similar deficit in habituation in schizophrenic patients.
It is now firmly established that anomalies in the P300 response are associated with a wide variety of psychiatric conditions,
including substance abuse. It has repeatedly been shown that the offspring of alcoholics demonstrate P300 amplitude
reduction despite their lack of exposure to alcohol, thus suggesting that this anomaly is an endophenotype tapping the
underlying genetic risk for alcoholism.
Research with this putative endophenotype also is helping to explain patterns of psychiatric comorbidity often observed with
other substance use disorders. To the extent that amplitude reduction indexes underlying genetic risk, the pattern observed in
the figure is consistent with the hypothesis that the covariation among these disorders reflects shared genetic influences.
There is ample evidence to support this notion, including twin and family studies showing that shared genes account for most
of the covariance among these disorders.
Consistent with the notion that P300 provides a neurobiological representation of the underlying genetic risk, P300 amplitude
also covaries with these disinhibitory disorders, with shared genes accounting for the association.
Because ERPs are derived from the EEG, it is possible to use time frequency analysis to identify the constituent EEG waves,
which, because they are time locked to the stimulus presentation, compose the ERP waveform. This type of analysis makes it
possible to determine the amount of each EEG frequency present at each point in time elapsing from the onset of a stimulus
to the resolution of the associated ERP. These event-related oscillations (EROs) can be partitioned into the same frequency
bands identified for spontaneous EEG, but these stimulus-elicited rhythms are likely to be functionally different from the
frequency bands that compose resting EEG. With respect to P300, specific neural activity have different responses during
elicitation of P300.
Event-related oscillations also are beginning to provide insights regarding brain dynamics and psychopathology, especially
regarding the development of drug dependence. Reduced delta and theta EROs have been associated with risk for the
development of alcoholism over and above the risk associated with reduced P300 amplitude, suggesting that they add
important predictive information not tapped by measures of the P300 endophenotype.
These EROs have been linked to gene variants involved in cholinergic and GABAergic neurotransmitter systems, systems
that have been implicated in the neurochemical pathways involved in substance use and P300 generation. Collectively, this
line of ERP/ERO research highlights the evolving potential of electrophysiological correlates of human information
processing to identify those at genetic risk for the development of alcoholism and related comorbidities.

-
Quote
In conclusion, the results of this study emphasize the importance of GABA–5-HT interactions (GABA - SEROTNIN RECEPTOR) and the role of these interactions in the pathophysiology of psychosis, dissociative states, and anxiety. gamma-aminobutyric acid deficits might predispose to the production or exacerbation of psychosis and perceptual alterations in the context of serotonergic activation, and this mechanism might apply to several disorders where GABA deficits have been described. Furthermore, the findings of this study lend support to the notion that dysfunction within a network involving several neurotransmitters might underlie the pathophysiology of psychosis and dissociative-like perceptual states.
Gamma-aminobutyric acid-ergic deficits might increase the vulnerability to the psychotomimetic and perceptual altering effects of serotonergic agents. These data suggest that interactions between GABAA and 5-HT systems might contribute to the pathophysiology of psychosis and dissociative-like perceptual states.

-
DISCLAIMER: My ex-girlfriend was advised by her money manager not to put $25,000 into my suggestion to buy stock in the company that was testing this drug. It was October 2012, and it was $2.00. She didn't tell me she was going to buy some, she did it on her own in case it went down to $1.000 and she lost money. (Great Girlfriend, I know). Money Manager guy said it was not wise. She decided not to. I sent a facebook message to close family members. Nobody would listen, and I have given 2 stock suggestions in my life: Netflix, NVIDIA (in 2008, whenever it split twice in Feb). I explained why I was so certain it was going to pop.
On my public Twitter account, I recommended it at 2.00. then at $4. $7. $9-11. All publicly, but I had no money and didn't realize how easy it would be to set up an investment account or I would have put at least 500 dollars in by selling everything I owned.
The 25,000 would have bought 12,500 shares and two years later was worth $500,000. My family wishes they listened.So...
I have been watching ACADIA since 2012, and although I had no money I recommended to wealthy family members and others to buy it at $2.00. I even publicly posted why. You can understand why it would appear on my radar right after finishing my degree and working on theoretical models and potential targets and I saw this.
I have not stopped watching ACADIA, and later did own stock option calls and because of financial issues sold them.
This is a very interesting drug. I knew it was going to get approved because the FDA needed a drug for Parkinson's, but I knew this was not the ultimate goal. The ultimate goal of a pharmaceutical company is to open up to a big market. Parkinsons as a target made it receive fast track status because no existing treatment for PD. Big institutional investors started getting in.
Risperdal causes issues (theorized and along with Yale's Souza lab and others in similar human research) that unlike regular schizophrenia, where these atypical antipsychotics block 5-HT2A sites, which means that in the one system we often talk about that has 5-HT2A inputs to produce GABA inhibitory signals would mean LESS GABA inhibition, the drug addressed both this and new method for working on the DOPAMINE system where the COMT theories and other targets for HPPD were coming out.
I designed a protocol study for HPPD using a pre-pulse inhibition design. I wrote out my theory for why this test would be useful and it ends there. I actually thought that it would be less helpful for pure HPPD visual symptoms, but most helpful for Depersonalization and Derealization symptoms. Maybe one day, we can get that study moving.
But, I have been linked to this drug for a long time, and I would like to see something come out of it. Don't believe the CNN hype articles, they were manipulation stories that are part of biotech investments .
-
-
I was rambling on, and then wanted a break and to come back to it. It is perfectly fine to comment. ") it gives a good look into my brain I think. Also, if I am going to discuss something that may put me in a precarious situation, I just hide it and come back to it later.
People with different learning styles or challenges in traditional classrooms or learning disorders are represented in a higher percentage than normal groups. This is Dr. Abraham's experience and I agreed. My qEEG and more specifically Dr. Frank Duffy's impression of my EEG back in 1999 is classic ADHD now. My front and central cortex has "astroundly high" amplitude for theta broadly across the region and even working on task, I am in this.high theta state. Of course, this is a state that monks are measured at achieving and people seek to reach this point with meditation. I can lucid dream almost at willner night if I thing about it for a few days. I can also see unusual connections in things and it has made what should have been an extremely lucrative stock trader. Howtoadhd in YouTube is a beautiful spirit with ADHD that has an wonderful channel she developed and has recently had other groups visiting on her channel.
I'll post something about this soon enough, but it may be a video.
Oh yes, my one point: more people with HPPD have these conditions, but do students feeling they are not working up to their own standards at school or life and are frustrated tend to take hallucinogens more than neurotypical and this is why the prevalence.
I take Adderall for it, and it is a life changer. I was in tears at all the first. I finally graduated college in 2011 after starting in 1996 and having three publications in the interim. But in 2008 I read a book without skipping pages. I am celebrating that Inhave not missed a doctor or dental appointment in one year using my Bullet Journal, which I treat with every reverence. I would miss final exams and appointments routinely and it could be written on my hand.
Ok, I have had trouble sleeping ever since I took a drop from 4 to 2mg of Klonopin recently and punctuated it with 7 days of klonopin free. I was in a safe space, so now I am trying 2mg and the day goes well, but sleep is not. This includes.that I have gabapentin to help. 20 years of benzos will definitely change expression of receptors, but I think we are much more resilient than we give ourselves credit for.
- dk
-
Mad Doc gives great advice. I can tell you that your choice of grammar for your post's subject already tells me -- I am recalling many years of people giving an introduction -- you said something that puts you in a group that has the best outlook.
What is it? You used exclamation marks, but just to say Hi. Not like "My life is ending!!!" But "New Here!!"
It may seem like a small observation, but if I have to make a judgement this is telling. It goes along with how well you are doing for your time frame and this is a great indicator.
- dk
-
Hi Thomz, I wish I could give you a great answer, but I can try and be reassuring and if you can tell more than it could help, but ultimately it will be you and a doctor that makes that decision.
1) Yes, the symptoms of HPPD may not appear until later in life, but typically it is much sooner than later. Also, research and personal experiences are pretty clear that alcohol is not a common if almost never a drug that starts HPPD after hallucinogen use.
2) Visual Disorders that share very similar symptoms, but the individuals have never taken a hallucinogen inside Visual Snow (this name is misleading, as the symptoms can include much more than the static snow symptom). Other disorders are best rule out by a Neurologist, but just to be complete with my answer I will mention Temporal Lobe Epilepsy.
3) Most people with HPPD will not question whether they have it or not after they have read the list of symptoms. It is such a shocking experience to hear someone talking about having their walls moving in the side of their vision but they never go anywhere or one day have perfect vision and the next day and beyond have blurred vision.
I hope that helps
-
I was going to write an introduction, etc. I don't have the energy now, but I do think it is VERY important that people with HPPD learn the truth about the amount of information that has existed out in the academic literature and why it frankly pisses me off that some researchers see that since 1969 there has been a stable disorder of symptoms that account for our condition, but they ignore it or don't have the time or desire to invest in researching what came before. I have read over 100 articles for my undergraduate thesis, and luckily had access to all of the databases I needed. So, I was privileged . Ii want to share that with you. I want to do these in videos, but I haven't set that up yet. So, here is the first major paper on HPPD that literally covers every major point and gets it right:
 Copy of horowitz_flashbacks (1).pdfCopy of horowitz_flashbacks (1).pdf
Copy of horowitz_flashbacks (1).pdfCopy of horowitz_flashbacks (1).pdf





-
 1
1
-
-
Hi viewers.
I would guess that many members have never experienced having me on the message board. A confluence of events occured that forced me away, and it has been hard to return.
Why you should read this because it will be a thread that will include information I never discussed before, I will provide information that had been withheld and I will open up the work I did that has been reviewed by members of Senior Commitees in the APA and senior researchers at Yale. They thought the research ideas where quite valuable.
My first admissions:
When my HPPD started and I developed panic attack disorder and was put on a high dose of Klonopin. For the last 10 years, I have been on 4mg a day.
A doctor finally had me tested, and I knew I have struggled with organization and my ability to control how I concentrate, and it was so severe I almost didnt graduate from High School, yet I slipped by as National Honor Society Preside t even though I failed all marling of Spanish, Calculus, Basic Accounting and Government.
I took 6 hours of tests. Part of the interesting parts are that I write essays at a 5th grade level when forced to use a pencil and paper. This was a strong contrast to my academic publications and the rest of my testing. The other area that surprised me, was that I scored in the SEVERLY IMPAIRED
Hagen, Moore,
Wickham, and Maples (2008) found that children who
have trouble with visual skills have difficulty with
attention, which interferes with executive brain
functioning and mimics ADHD symptoms. Children
with VPD may be easily distracted by too much visual
stimulation. -
I have a research study protocol designed to test aspects of this. The brain handles the compensation of the excess signals to help you adapt to your environment.
First, wearing Sunglasses is one of the great pieces of advice that I cant stress enough. Blue blockers and anti glare can reduce the amount of stimuli reaching your eye, which dampens the range of signal strength you brain has to process
For example, a Strobe Light in a Dark Space is AWFUL. This is from the rapid cycling of strong on signal and off signal.
In bright Sunlight, when I am reading a book with the Sun against my back, on many occasions the black text turned green as bright green ink.
Some users hate the darkness, and the reason is similar in theory. When the brain is not receiving visual information, if it expects something or is overactive it will create images and/or this is a time it is easiest to focus k the symptoms. I would cry, and beg just to see a plain black wall. As it stands, I am not counting on that happening, but this is one line of research I whole like to explore.
This is one invoice for a purchase I was readying for research.
-
Since it started, I thought the Nationbuilder system had some very unique things that can work with another system to create a very effective tool for generating interest, policy and awareness with a very powerful human and other management side.
It worked for the Prime Minister of New Zealand, and many large non profits are switching over.
It enables EU privacy rules downloadable information files and because it is used election sites it is very conscious about security.
I am currently testing just a simple sign up system, which will ask for a phone number and an address, the phone number is mandatory, and it will let you know I will be in touch with you. We could also make it where it could sign someone up for events, get information. In the backend, someone texting the message to this main number will have an account created, and I have a dashboard of tasks to do and it will pop up I need to contact you. I set up auto tags so I know supporters, it can set up memberships, be useful for doctor recommendations or even send a phone text alert if research or a social group is set up in your region (maybe a 100 mile radius). It works world wide.
It can collect money, but full disclosure is that it goes straight to my bank account. I used to have a seperate 501(c)(3) but dissolved it after the research and life happened.
So, if you want to just test the basic system, I also have it set up to give any user 12 months of free "Subscriber" level membership. Again, full disclosure, this is essentially had no meaning at this point, and I never wanted to offer people unable to pay for services any denied services, but it could mean that my library of documents that cost money can be accessed with a controlled system.
The themes use liquid and are rather simple. I was an ASP and C programmer back in 1996 and then did PHP with a MySQL server and designed a research system to pass Mt. Sinai School of Medicine New York IRB requirements and successfully had 384 participants and is currently one of the most cited papers for DPD diagnostic criteria (almost or over 100 citations) and we did it without a budget.
Here is the test signup text:
Text HELP to +17346071765 to be an early tester or the contact system. I will call you back within 2 days and explain much more.
For donations, until I point a domain to the site we have only the subdomain. I own eyedisorders.org, hppdonline.com, and perceptualpsychology.com.
If you are interested learning more, and about what server host I prefer to use if not this place and the VPS and other plans they have and mu history with them I can point you in that way. Knowing the best way to have OPENauthentication so the systems are happy communicating but without forcing Twitter or Facebook accounts is a big goal.
I need people to help support me, and I had a major break through in my personal life and am down in my meds and grad school is next goal and I have new protocols for visual neuroscience and imaging testing. Also, epidemiological tests. There are very smart people on here, and very capable people that can do everything from missile guidance systems, very prestigious attorneys and software folk.
Time to get back in the saddle --- just so much bad information -- and we should control our story.
https://davidkozin.nationbuilder.com/early_donors
Current design:
Also, as a gift:
-
1 hour ago, Jay1 said:
Yea, i've tried pretty much everything that's ever been mentioned on this forum! Nothing works for me, sadly.
Yes, Jay is doing pretty damn well considering. So, if managing the board, paying for it and regular life successfully is a measure of success handling the disorder than I think Jay is doing quite fine. However, visuals are probably just as they were a few years back.
- dk
-
This is a good list.
I am setting up the space where people with HPPD, their allies or medical professionals can use to look up information about the big questions:
What pharmacological treatments have evidenced based positive results? What medications are specifically CONTRAINDICATED for individuals with HPPD?
The page would have 30 or so medications I would imagine. It could be broken down into a Professional and a Consumer Page. I think it would be nice if a more advanced write up with citations were included as a Continuing Medication Education "type" certification, which a licensed medical professional can take in order to be listed on the World Map with their information as a doctor that at minimum has familiarity with the most important concepts.|
The goal of the web site is to create the most value and impact with the little money that we have. If individuals with HPPD go to one of these doctors, and the doctor does not prescribe risperidone as a first line of defense because the web site details a very outspoken research and patient community about why this class of anti-psychotics will produce an increase in symptoms.
Imagine saving 5 people from having to experience this awful period, which I have known some people to have been hospitalized and placed on anti-psychotics, and as the symptoms got worse they prescribed more antipsychotics. It was about 6 months or maybe a year later, the medication was stopped and the symptoms were dramatically improved. This is where everyone can have an impact.
-
 2
2
-
 3
3
-
-
-
I will get into this in a person message, but to be short:
They are using it on an Amazon server if I had to guess.
The issues are:
1) I created a message board system in 1998, then I used early versions of PHPBB and eventually SMF. I have hosted the web site since 1998, and the most traffic the site received was between 2001-2004? I eventually ended up with a managed dedicated server. Honestly, this was a waste of money.2) HPPDonline.com has cost $30 for over 20 years. Hosting cost about $200/month for about a two year period while hosting the research for Depersonalization disorder and heavy traffic.
3) Hosting has cost $7,000 over that period.
4) I have two goals for research that must be maintained for the web site (If I want to use it as such), but either way I refuse to have anyone other than myself or Jay have access to the actual database. As it is, we have have moderation action logged, every wrong login from an Admin marked and because 9 our of 10 members do not sign in, and I know a lot of them because risking even having any meta data connected to HPPDonline.com and your workplace, spouse, partner, etc (in many more cases that the younger generation might actually appreciate) would mean people would get fired, divorced and just for finding a job for those of us with public front "ends": I am unable to find any normal work. Every hiring agency runs a Google search at minimum. The Harvard and publication work only works FOR me if I am applying for a position that requires me to be a researcher. Other that this, would you hire someone you didn't know to process you data entry if over 20,000 pages on Google link to this new employees name to drug use, tripping and why are they applying here?
5) SO, I AM VERY PROTECTIVE ABOUT THE DATABASE. It is also information that gets included in a write up for a grant. Writing, "Limesurvey is hosted on Little Jimmy's Server Appliance in his bedroom next to his EZ Bake Oven and the family's alcohol" just won't make it as good as 24/7 Linux Engineers, with multiple datahousing centers and data storage compliance is XXXXXX, including Carbon Offsetting XXXXX".
6) So, I am going to ask the people who run the hosting for Joomla's own sites if they have experience pulling from Invision Power Web databases and importing it, and put on one of their plans that do not use hyperbole and I can e-mail the tech's at the firewall if I want to create my own rules/etc. The owner of 15+ years still works with others on the floor. The host is https://www.rochen.com/
Any discussion I am open to hear, but need blood and sweat to be convinced otherwise. Rochen has edited PHP and other scripts as part of normal support while I was caught in a jam. The support is amazing.
We could all pay for it with a cryptocurrency donation. BAT coin? Using Brave server.
Anyway,. I would also need some people for developing static web pages.
If you want a history of HPPDonline.com... check out the Internet Archives.
HPPDONLINE.COM OVER THE AGES: -
It was a spike for 1 month. and dropped already back to normal. I have a few ideas, but one part is I hate that I lost the ability to access the raw database files without having to ask for them.
Maybe a paradigm shift for the whole community? But, after we have the information in our hands only, store off cloud (i took like it on an Amazon server. There are people expressing interest in writing static content, but I just don't want to loose the research and info aspect. We do have hppdonline.com and can point it wherever, but should wait until we take the stuff with us.
I have to pick up family from train station today, cleaning house and I am moving back from a temporary living situation while handling the medication withdrawal, and now that I have jumped down I will have a new phase.
- dk
-
Ok, so 32 members last posted between and
It is possible because of the facesofhppd info, but I am still annoyed with invision to require such a jump.
- dk -
Ok, the the database format that invision users and the conversion scripts to put it on a different message board service is going to require importing. I have a special love for Rochenhost as a private host service that hosts Joomla's official site.
I won't let anyone host the site at their home or private server unless I have known you for 15 years and you have remarkable credentials with the community. It is a HUGE responsability to hold the email addresses and private messages access of all of the people on this web site who want to keep it private, and I wouldn't host it on a server that I own, but a VPS or equivalent.
But, I knew invision would start screwing us over. I doubt traffic jumpted like.
They don't offer enough to be worth it.
Jay, I trust you with a copy of the sql db files in holding. I am going to do the same and see what the issue is with getting it converted to another open source service, or hell... maybe we take a radical shift and lock the database and talk about what are our next steps. Either way, is someone willing to help Jay out.
I will offer all I can, which is my time to the donor. - I will see how bad the situation is (and suggestions).
I am going to get my Reseller Plan at Rochenhost open for my own purposes.
https://www.rochen.com/reseller-hosting/
People who know, know. Unless you work for a datacenter and will sign your name away to one of our attorney's for an NDA, and we do have a ton of HPPD attorneys with serious credentials. Anyone who would host it would be required to treat it like a research database with a ton of information that is worth less stress that it is worth.
Ok, I am writing a reactionary message. I literally am glad I got this today and not the last 10 days of a klonopin withdrawal designed to bring be down to the lowest dose I have had in 10 years. I am going pretty good after breaking through and right now. 4mg to 1mg. After 20 years.- dk
Ok, the the database format that invision users and the conversion scripts to put it on a different message board service is going to require importing. I have a special love for Rochenhost as a private host service that hosts Joomla's official site.
I won't let anyone host the site at their home or private server unless I have known you for 15 years and you have remarkable credentials with the community. It is a HUGE responsability to hold the email addresses and private messages access of all of the people on this web site who want to keep it private, and I wouldn't host it on a server that I own, but a VPS or equivalent.
But, I knew invision would start screwing us over. I doubt traffic jumpted like.
They don't offer enough to be worth it.
Jay, I trust you with a copy of the sql db files in holding. I am going to do the same and see what the issue is with getting it converted to another open source service, or hell... maybe we take a radical shift and lock the database and talk about what are our next steps. Either way, is someone willing to help Jay out.
I will offer all I can, which is my time to the donor. - I will see how bad the situation is (and suggestions).
I am going to get my Reseller Plan at Rochenhost open for my own purposes.
https://www.rochen.com/reseller-hosting/People who know, know. Unless you work for a datacenter and will sign your name away to one of our attorney's for an NDA, and we do have a ton of HPPD attorneys with serious credentials. Anyone who would host it would be required to treat it like a research database with a ton of information that is worth less stress that it is worth.
Ok, I am writing a reactionary message. I literally am glad I got this today and not the last 10 days of a klonopin withdrawal designed to bring be down to the lowest dose I have had in 10 years. I am going pretty good after breaking through and right now. 4mg to 1mg. After 20 years.- dk
-
Yes. the researcher is stating their desire to advance research into these drugs. However, a biased researcher wanting glowing reports about people tripping then having great lives would NOT advertise their survey on this web site.

Hey Hope1, I was just putting up the results of the new HPPD survey while reading your post, and a Master's degree thesis is a recent graduate with a Bachelor's and I have a soft spot for this group.
The researcher could just as easily be a person with HPPD, and asking this question:There question the researcher is asking:
More specifically I am conducting research to understand the long term effects of psychedelic drugs by exploring whether there are differences between the perceived well-being, life satisfaction and mood of psychedelic drugs users and non-psychedelic drug users.
So, the experiment: Is there a significant different between the perceived well-being, life satisfaction and mood between people who take psychedelics differ than non-psychedelic drug users.
So, Hope1, you are a psychedelic drug user. You would probably answer very negatively on all of these areas. You would probably be way down at the bottom. But, by including HPPD individuals in the test, it allows for a representative sample to be included that (on face value) would have negative results (generally).Generally, assuming the basic premise is as stated, research design would ask if a person has HPPD or ask questions that would inform that a person does, and use item response theory techniques to look to see if answers are highly predictable based on association with HPPD (i.e. participants that marked that they received an HPPD diagnosis could predict a person's overall score more than any other question). This should not invalidate the responses, but this becomes part of the discussion and also advanced statistical techniques can help control for this.
I have not checked up on this student and their adviser, but I think it is good science to develop a protocol to include advertising the survey on sites where people have a majority of likely negative responses while probably advertising on sites like Erowid or others that would skew towards the positive.
But, for feel good news:I agreed to put my name on research with a conclusion that MDMA did not show significant negative side effects for a large battery of neurocognitive tests because I thought the design with the control groups was smart, I created the database of responses for import into the statistical software (lots of numbers), spent some of my best hours sitting next to one of the top 10 psychiatric researchers of the century discussing the results and statistical methods to investigate the responses and worked on part of the manuscript related to my work.
It doesn't look good on my HPPD resume, but I dare someone in the pro-psychedelic community or any research community to claim I am biased against psychedelics/enactogens, and when I do talk about the negatives and HPPD then my opinion is easier to digest without judging me as biased against psychedelics. So, I hope when I ask for research participants with the visual snow group that I don't receive a strong backlash against research because some very vocal visual snow folk have fought with me over VS having nothing to do with HPPD. The rationale was because HPPD is defined by requiring a hallucinogen, so I argued that the definition is made by humans and I know them and I know how the DSM is made and it could very well be called Altered Perception Disorder, Hallucinogen onset vs APD, not otherwise specified. However, it was an emotional argument, so I left. The point that the DSM diagnosis are often not based on a biological reality or a proven etiology, and at the time they were biased so that when 1 psychiatrists sees a patient and diagnose them with HPPD then 9 others would make the same diagnosis independently. The phrase, to cast a wide net, would apply to the methods for creating a diagnosis. The content validity of this diagnosis was sacrificed so that the diagnosis would be reliably reproducible. In many other diagnostic entities this was fixed, but until the last few years HPPD has been the ugly duckling forget about them group. Dr. Abraham is retired. He was the one sending in tons of information to prove otherwise. This is why I am so excited that my plans and a few other researchers are coming together at the right time.
I am sure you saw it, and I have this feeling (ok, I was watching the server processes queue and it looked more like a certainty) that anyone that listed a desire to be notified about research or perhaps (be notified about anything at all on this site) received an email about the Faces of HPPD research that is both published in an academic journal and Dr. Lewis's wisely had the graphics of the main conclusions available for the community without having to violate copyright.
So, if you missed that, check out: -
Faces of HPPD Infographic - Lewis, Doreen M. PhD
View FileHPPD RESEARCH SURVEY RESULTS!
Link to Article: Post-
Submitter
-
Submitted06/14/2019
-
Category
-
-
Of course, I am not happy with reckless research. Jay and others then usual me after they did, with questions and verification of the research methods, and I look who is doing it and I usually know if there is or is not good science coming from the lab.
I have yet to check this, and I am here because I was speaking with a reseacher about HPPD and some unique factors that may shed see insight into this area. So, I opened this thread up.
I am not going to police behavior, but in the medical and research community the fanatics are the first not to be taken seriously. Tim Leary did little to help their cause.
In 2004ish, A prominent German researcher said to me, "I have read countless years of research with LSD, and have yet to find one case about HPPD. He had good reasons in his mind to think I was full of shit. HPPD is not dose dependent and it isn't always on the first time, but maybe the 64th time. Millions of people have taken LSD, so why have I not heard of it. "
He did do a tremendous amount of research. He was not acting in bad faith. I told him, honestly, I can't explain these things and it bothers me also. I can't say with 100% certainty that I didn't get infected by a parasite that day. But, what I can say, is I have over 1000 people who come from backgrounds in the military, legal, medical, students, caretakers, teenagers, teachers, members of our government and more that I have spoken with and we all share the same symptoms and all attribute it to the same type of event and we all react paradoxically to drugs like Risperdal. I can tell a person on the phone to not tell me about their symptoms, but I will tell them what they see before they say a word, and I have for some of you. So, all I can say to this researcher is open your mind at least to it being real and one major causal agent is hallucinogens like LSD.
His email said, I can't argue with a level headed response like that. You are willing to question it yourself, but statistically and in your experience it would ridiculous to think otherwise. I believe you.
A few years later a case report and discussion comes out and a first case of HPPD published with a new psychadelic and he is the first name.
Another researcher, very intelligent and one of the most influential in psychadelic research was embarrassed when they saw my bibliography of studies. But, I didn't get an audience with them because I told him he was doing the wrong thing, because I was not one of the people that asked to get treated.
I am giving HPPD people the most grief because our actions are what helps control our boat. I made a few bad decisions, and because of my influence it affected us all. When I am sending out applications and talking with researchers, the Lab I work in might just be doing pro-psychadelic work because our areas and needs might be very closely aligned. Until proven otherwise, nobody is an enemy. Potential allies.
Jay is 100% correct. The largest study to characterize HPPD so far, which was published in a Drug & Alcohol Research Journal. The authors include Earth & Fire Erowid, two people that provided me excellent advice and also a very comprehensive review of HPPD.
Also, some of my biggest allies that have spoken out and discuss with my cases of HPPD include leaders in their field of psychedelic research.
Honestly, if I had to take the statistical odds and I was not a person with HPPD but I did have PTSD from combat, when the choice is between taking an SSRI and maybe an antipsychotic for my life (perhaps develop tremor) or take two pills of MDMA with certified therapists with use of these substances, then I would choose the MDMA. MDMA has been a tremendous tool for PTSD, BUT I would also want as a patient to have an informed consent form and a researcher that can talk to me about the realistic risks of HPPD. Perhaps, they ask if I took mushrooms: would you agree that you can take much less mushrooms and trip just as hard as your friends? I know this was my case, and perhaps it is 70% of the cases. Then, this would be a disqualifying item for participating in research.
Psychedelics help cluster head suffers. This is literally the only pain so severe that a person without any psychopathology have killed themselves just to end the pain They come in clusters, injections of Heroin would not help. They are nickbamed uicide headaches and I have witnessed them and I would probably ripy eyes out before going through them all my life. But, somebers started finding that mushrooms aborted an entire yearly cycle more.
As a community, we have been prejudged as malingers, people faking a disorder or just people with normal symptoms but we are just paying to much attention to them. Where have I gotten the biggest pushback? Anti-drug people. I have received calls from people at a conference after they spoke to a NIDA representative who called HPPD most like malingers. My earliest allies, where the people who were on the front lines.
It does suck when research is not going your way with funding. Look at Visual Snow Initiative. They have put a few 100,000 in research labs hands and the executive director/founder is a development and messaging genius.
Hey, but like Greg and I would do back in 2002: a drunken post comes out and swears I am stealing money or because I had a section on the website for current drug users worth HPPD to write messages because it is triggering to average users, then I was enabling and swearing. Then, I fight back. Next day, all is good and usually apology about writing messages at 4 AM when in a bad mood.
Hug a psychadelic researcher, because they just may be the person that secures you funding because the argument they should help with funding because nderstanding HPPD will prevent a possible catastrophic participant experience that could threatren all of their research future may just be on someone's mind.
I am still out and personal medical issues outside of HPPD. I stopped making promises until I do something new.
David, Actual
-
Thanks Jay! I encourage participation with the study. If a tenth of the HPPD members I have spoken to participated, the sample size would be comparatively large and this would be helpful (at least would not hurt) for getting additional research and large valid sample sizes (in theory) increase the significance of statistical measures.
- dk
-
Hi Everyone. I read through the Informed Consent and sent an e-mail to the study researchers just to verify authenticity and the Lab.
I will follow up when I receive a response. The extra caution is because of the new account (even if others know about or are participating with the study).
David
For the researchers use per my email: 23011974300
-
References
Abraham, H. D. (1980). Psychiatric illness in drug abusers. The New England Journal of Medicine, 302(15), 868-869.
Abraham, H. D. (1982). A chronic impairment of colour vision in users of LSD. The British Journal of Psychiatry : The Journal of Mental Science, 140, 518-520.
Forty-six users of the hallucinogen lysergic acid diethylamide were compared with 31 controls on a test of colour discrimination an average of two years after their last exposure to the drug. Controls performed better than users, and LSD users without flashbacks performed better than users with flashbacks. An analysis of variance between the three groups was significant at P less than 0.001. This study suggests that some users of LSD may have a sustained or irreversible impairment in colour discrimination.Abraham, H. D. (1983). L-5-hydroxytryptophan for LSD-induced psychosis. The American Journal of Psychiatry, 140(4), 456-458.
The serotonin precursor L-5-hydroxytryptophan reversed the symptoms of a 23-year-old man suffering from LSD-induced psychosis who participated in a randomized, double-blind crossover study of the drug and a placebo. This finding is compatible with the speculation that some LSD-induced psychotic disorders may be caused by a relative deficiency of CNS serotonin.Abraham, H. D. (1983). Visual phenomenology of the LSD flashback. Archives of General Psychiatry, 40(8), 884-889.
One hundred twenty-three persons with a history of LSD use were studied for the presence of the LSD flashback phenomenon and compared with 40 control subjects. A syndrome emerged that included ten distance visual disturbances. It had lasted for five years in half of the population, was treatable with benzodiazepines, exacerbated by phenothiazines, and precipitated by 19 different stimuli, most commonly emergence into a dark environment. Sensitivity to LSD as determined by flashbacks appears to divide the study sample into three discrete subgroups. There may be a genetic basis to LSD sensitivity.Abraham, H. D. (1989). Stimulants, panic, and BEAM EEG abnormalities. The American Journal of Psychiatry, 146(7), 947-948.
Abraham, H. D., & Aldridge, A. M. (1993). Adverse consequences of lysergic acid diethylamide. Addiction (Abingdon, England), 88(10), 1327-1334.
The continued endemic use of hallucinogenic drugs, and of LSD in particular, raises concern regarding their short and long term adverse consequences. The epidemiology of LSD abuse is reviewed suggesting an increase in LSD use among the young as the prevalence rates for other substances continues to fall. Evidence supports the association of LSD use with panic reactions, prolonged schizoaffective psychoses and post-hallucinogen perceptual disorder, the latter being present continually for as long as 5 years. Evidence does not support claims of genetic disorders arising from hallucinogens. In light of the foregoing, current data confirm earlier findings of long lasting psychopathology arising in vulnerable individuals from the use of LSD. A hypothetical long term molecular mechanism of adverse effects is proposed.Abraham, H. D., Aldridge, A. M., & Gogia, P. (1996). The psychopharmacology of hallucinogens. Neuropsychopharmacology : Official Publication of the American College of Neuropsychopharmacology, 14(4), 285-298. doi:10.1016/0893-133X(95)00136-2
Hallucinogenic drugs have been inhaled, ingested, worshipped, and reviled since prehistory. With the purification and synthesis of bontanical preparations and the ensuing discovery of chemically unique agents, hope was raised regarding their therapeutic potential, but this hope has been clouded by an epidemic of abuse and an inventory of adverse effects. This review examines aspects of that controversy, including the history of hallucinogens, epidemiology of current hallucinogen abuse, the association of LSD use with prolonged psychoses and hallucinogen persisting perception disorder, and the efforts to demonstrate the drug's therapeutic efficacy. Human subject ramifications in hallucinogen experimentation are discussed. Future lines of research are suggested in human, animal, and tissue culture paradigms.Abraham, H. D., & Duffy, F. H. (1996). Stable quantitative EEG difference in post-LSD visual disorder by split-half analysis: evidence for disinhibition. Psychiatry Research, 67(3), 173-187.
Hallucinogen persisting perceptual disorder (HPPD) may follow the ingestion of LSD or other hallucinogens in a subset of users. It is characterized by chronic, intermittent or constant visual hallucinations of many sorts persisting beyond the period of acute drug effects. We studied 44 LSD-induced HPPD subjects and 88 matched controls to search for spectral and evoked potential differences using quantitative EEG (qEEG). HPPD subjects demonstrated faster alpha frequency and shorter VER (visual evoked response) latency, consistent with prior animal and human data on response to acute LSD administration which suggest LSD-induced cortical disinhibition. AER (auditory evoked response) latency was prolonged consistent with a differential LSD effect upon visual and auditory systems. The exploratory T-statistic significance probability mapping (T-SPM) technique demonstrated HPPD-control differences mostly involving temporal and left parietal scalp regions, confirmed by a split-half analysis. Significant variables were all derived from the long latency flash VER and click AER. None were derived from spectral analyzed EEG data. Canonical correlation between SPM-derived measures and variables reflecting disease severity was highly significant. A between-group stepwise discriminant analysis based upon a full set of qEEG measures demonstrated 87% prospective classification success by jackknifing and 88% success in a separate split-half analysis.Abraham, H. D., & Duffy, F. H. (2001). EEG coherence in post-LSD visual hallucinations. Psychiatry Research, 107(3), 151-163.
LSD use in certain individuals may result in chronic visual hallucinations, a DSM-IV syndrome known as hallucinogen persisting perception disorder (HPPD). We studied 38 HPPD subjects with a mean of 9.7 years of persistent visual hallucinations and 33 control subjects. Measures of local and medium distance EEG spectral coherence were calculated from all subjects. Coherence, a measure of spectral similarity over time, may estimate cortical coupling. In the eyes-open state in HPPD subjects, widespread reduction of coherence was noted. However, upon eye closure, the occipital region demonstrated augmented regional coherence over many frequencies but with reduced coherence of the occipital region to more distant regions. This occipital coherence increase correlated with previously reported shortened occipital visual evoked potential latency for HPPD subjects. We speculate from coherence and known clinical and psychophysical data that, in HPPD, there is widespread cortical inhibition in the eyes-opened state, but localized and isolated occipital disinhibition upon eye closure, a state known to facilitate hallucinatory experiences. An analogy is drawn to findings in the interictal and ictal epileptic focus. In HPPD, we speculate that occipital EEG hypersynchrony resulting from increased regional coherence, when coupled with relative isolation of visual cortex, especially upon eye closure, facilitates hallucinations and illusions.Abraham, H. D., & Mamen, A. (1996). LSD-like panic from risperidone in post-LSD visual disorder. Journal of Clinical Psychopharmacology, 16(3), 238-241.
Risperidone, a novel antipsychotic agent, is an antagonist of postsynaptic serotonin-2 and dopamine D2 receptors. In certain individuals, the hallucinogenic drug lysergic acid diethylamide (LSD) is associated with apparently lifelong continuous visual disturbances, characterized in DSM-IV as hallucinogen-persisting perception disorder (HPPD). Because the hallucinogenic mechanism of LSD is known to act in part at postsynaptic serotonin-2 receptors, it is noteworthy that three HPPD patients treated with risperidone reported an exacerbation of LSD-like panic and visual symptoms. We conclude that HPPD may be a relative contraindication for the use of risperidone.Abraham, H. D., & Wolf, E. (1988). Visual function in past users of LSD: psychophysical findings. Journal of Abnormal Psychology, 97(4), 443-447.
Adamczyk, D. T. (1996). Visual phenomena, disturbances, and hallucinations Optometry Clinics : The Official Publication of the Prentice Society, 5(3-4), 33-52.
The visual system and its processing of sensory information can be affected in a variety of ways that may be either normal or associated with numerous disorders and diseases. Visual images produced by the intrinsic components of the eyes are often normal and are known as entoptic phenomena. In contrast, the visual system may be disrupted by various disorders and pathologic processes, which can result in metamorphopsia, transient loss of vision, and positive scotomas. Such disruptions can be secondary to retinal and optic nerve disease, migraines associated with visual auras, and cerebrovascular and neurologic diseases; they can also be side effects of certain drugs. In addition, the visual system may process incoming sensory information in such a way that what is seen is perceived incorrectly, i.e. illusion; or the visual system may produce images of things not really there, i.e. hallucination. Various types of visual phenomena, disturbances, and hallucinations are discussed. The numerous visual presentations need to be differentiated so that appropriate treatment, management, and patient education can be rendered.Alarcon, R. D., Dickinson, W. A., & Dohn, H. H. (1982). Flashback phenomena. Clinical and diagnostic dilemmas. The Journal of Nervous and Mental Disease, 170(4), 217-223.
The study of flashback phenomena has been neglected in recent years. A case study and a subsequent literature review examine areas about which conflicting opinions exist. Epidemiological studies have not arrived at universally acceptable classificatory schemes. Clinical approaches vary in accounts of phenomenology of the syndrome and the typology of personalities involved. Etiology remains unknown in spite of numerous theories, most of them not experimentally tested. Diagnostic studies may benefit from recent technological advances such as continuous electroencephalogram, computerized axial tomography scan, cerebral blood flow, and neuropsychological tests. The Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition, does not seem to provide an adequate taxonomic niche for this disorder. Therapeutic interventions are examined and their results critically analyzed.Alcantara, A. G. (1998). Is there a role for the alpha2 antagonism in the exacerbation of hallucinogen-persisting perception disorder with risperidone? Journal of Clinical Psychopharmacology, 18(6), 487-488.
Aldurra, G., & Crayton, J. W. (2001). Improvement of hallucinogen persisting perception disorder by treatment with a combination of fluoxetine and olanzapine: case report. Journal of Clinical Psychopharmacology, 21(3), 343-344.
Assmus, H., & Reimer, F. (1972). Accidental LSD intoxication in three siblings with flashback. [Akzidentelle LSD-Intoxikation bei drei Geschwistern im Kindesalter mit Nachhallpsychose (Flashback] Praxis Der Kinderpsychologie Und Kinderpsychiatrie, 21(6), 207-209.
Barlow, H. B., & Sparrock, J. M. B. (1964). The Role of Afterimages in Dark Adaptation. Science, 144(3624), 1309-1314. doi:10.1126/science.144.3624.1309
Barron, S. P., Lowinger, P., & Ebner, E. (1970). A clinical examination of chronic LSD use in the community. Comprehensive Psychiatry, 11(1), 69-79. doi:DOI: 10.1016/0010-440X(70)90206-3
Benneyworth, M. A., Smith, R. L., Barrett, R. J., & Sanders-Bush, E. (2005). Complex discriminative stimulus properties of (+)lysergic acid diethylamide (LSD) in C57Bl/6J mice. Psychopharmacology, 179(4), 854-862. doi:10.1007/s00213-004-2108-z
RATIONALE: The drug discrimination procedure is the most frequently used in vivo model of hallucinogen activity. Historically, most drug discrimination studies have been conducted in the rat. With the development of genetically modified mice, a powerful new tool has become available for investigating the mechanisms of drug-induced behavior. The current paper is part of an ongoing effort to determine the utility of the drug discrimination technique for evaluating hallucinogenic drugs in mice. OBJECTIVE: To establish the training procedures and characterize the stimulus properties of (+)lysergic acid diethylamide (LSD) in mice. METHODS: Using a two-lever drug discrimination procedure, C57Bl/6J mice were trained to discriminate 0.45 mg/kg LSD vs saline on a VI30 sec schedule of reinforcement, with vanilla-flavored Ensure serving as the reinforcer. RESULTS: As in rats, acquisition was orderly, but the training dose was nearly five-fold higher for mice than rats. LSD lever selection was dose-dependent. Time-course studies revealed a rapid loss of the LSD stimulus effects. The 5-HT(2A/2C) receptor agonist, 2,5-dimethoxy-4-bromoamphetamine [(-)DOB] (1.0 mg/kg), substituted fully for LSD and the 5-HT(1A) receptor agonist, 8-hydroxy-2-(di-n-propylamino)-tetralin (8-OH-DPAT) (1.6 mg/kg), substituted partially for LSD. Pretreatment with the 5-HT(2A) receptor-selective antagonist, MDL 100907, or the 5-HT(1A)-selective antagonist WAY 100635, showed that each antagonist only partially blocked LSD discrimination. Substitution of 1.0 mg/kg (-)DOB for LSD was fully blocked by pretreatment with MDL 100907 but unaltered by WAY 100635 pretreatment. CONCLUSIONS: These data suggest that in mice the stimulus effects of LSD have both a 5-HT(2A) receptor and a 5-HT(1A) receptor component.Benneyworth, M. A., Smith, R. L., & Sanders-Bush, E. (2008). Chronic phenethylamine hallucinogen treatment alters behavioral sensitivity to a metabotropic glutamate 2/3 receptor agonist. Neuropsychopharmacology : Official Publication of the American College of Neuropsychopharmacology, 33(9), 2206-2216. doi:10.1038/sj.npp.1301600
Recent clinical studies in schizophrenic patients show that a selective agonist of group II metabotropic glutamate (mGlu) receptors has robust efficacy in treating positive and negative symptoms. Group II mGlu receptor agonists also modulate the in vivo activity of psychotomimetic drugs, reducing the ability of psychotomimetic hallucinogens to increase glutamatergic transmission. The use of mouse models provides an opportunity to investigate the dynamic action that mGlu2/3 receptors play in regulating the behavioral effects of hallucinogen-induced glutamatergic neurotransmission using genetic as well as pharmacological strategies. The current study sought to characterize the use of the two-lever drug discrimination paradigm in ICR (CD-1) mice, using the hallucinogenic 5-HT2A/2C receptor agonist (-)-2,5-dimethoxy-4-bromoamphetamine [(-)-DOB)] as a stimulus-producing drug. The (-)-DOB discriminative stimulus was dose-dependent, generalized to the hallucinogen lysergic acid diethylamide, and was potently blocked by the 5-HT2A receptor antagonist M100907. However, contrary to our prediction, the hallucinogen-induced discriminative stimulus was not regulated by mGlu2/3 receptors. In a series of follow-up studies using hallucinogen-induced head twitch response and phencyclidine-induced hyperlocomotion, it was additionally discovered that the repeated dosing regimen required for discrimination training attenuated the behavioral effects of the mGlu2/3 receptor agonist LY379268. Furthermore chronic studies, using a 14 day (-)-DOB treatment, confirmed that repeated hallucinogen treatment causes a loss of behavioral activity of mGlu2/3 receptors, likely resulting from persistent activation of mGlu2/3 receptors by a hallucinogen-induced hyperglutamatergic state.Bergamin Oliver, Schoetzau Andreas, Sugimoto Keiko, & Zulauf Mario. (1998). The influence of iris color on the pupillary light reflex. Graefe's Archive for Clinical and Experimental Ophthalmology, 236(8), 567-570.
· Results: Iris color (blue vs brown) influenced statistically significantly (P · Methods: Pupil perimetry was performed on 50 healthy volunteers with the Octopus 1-2-3 automated perimeter. Within the 30-deg visual field 33 test locations were investigated four times. Stimulus parameters were Goldmann size V (1.72°) intensity 1632 cd/m2 stimulus time 200 ms background illumination 0 cd/m2 and interstimulus interval 3 s. Pupillometric parameters studied were initial pupil size amplitude (magnitude of pupillary contraction) latency time contraction time pre-PLR movement contraction velocity parameters were investigated by analysis of variance by the independent variables blue and brown irides. · Background: This study was carried out to investigate the effect of iris color on the pupillary light reflex (PLR) in normal healthy volunteers. Abstract<· Conclusions: Pupillary contraction amplitude and velocity depended on iris color whereas pupil size and latency time were independent of iris color. Therefore iris color might be considered when evaluating pupillary movements in pupil perimetry. 0.05) amplitude (0.504 mm vs 0.594 mm) contraction time (401 ms vs 407 ms) contraction velocity (13.75 mm2/s vs 16.01 mm2/s) and redilation velocity (4.80 mm2/s vs 5.66 mm2/s). Iris color did not influence initial pupil size (4.78 mm vs 4.83 mm) latency time (520 ms vs 521 ms) (0.328 mm2/s vs 0.325 mm2/s).Bone Pina, I., Ramos Gorostiza, P., Villalba Yllan, P., & Valle Fernandez, J. (2000). Persisting and late onset psychotic disorder due to consumption of ecstasy (MDMA). [Trastorno psicotico persistente inducido por consumo de extasis (MDMA)] Actas Espanolas De Psiquiatria, 28(1), 61-65.
Let us present a case of recurrent paranoid psychotic episodes in a patient with a history of abuse of > (MDMA: 3, 4-methylenedioxymethamphetamine), that persisted after a long withdrawal time, that, in our opinion, after an exhaustive differential diagnosis, may be attributed to that consumption. The carachteristics of this case are formally and naturally equivalent to those referred to in other papers about paranoid psychosis after abuse of MDMA, in which the sudden appearance, and the symptomatolgy of an intense feeling of threat and physical violence outstands, accompanied by abnormal corporal perceptions. In the case hereby presented, the withdrawal time is longer than that described in other publications. Even though in some authors' opinion this should be considered as comorbility or dual diagnosis, in our opinion enough facts exist suggesting that this is not a case of functional mental disorder but an organic disorder secondary to the neurotoxic effect of MDMA.Cooper, H. A. (1955). HALLUCINOGENIC DRUGS. The Lancet, 265(6873), 1078-1079. doi:DOI: 10.1016/S0140-6736(55)91156-9
Cummings, J. L., & Miller, B. L. (1987). Visual hallucinations. Clinical occurrence and use in differential diagnosis The Western Journal of Medicine, 146(1), 46-51.
Visual hallucinations occur in diverse clinical circumstances including ophthalmologic diseases, neurologic disorders, toxic and metabolic disorders and idiopathic psychiatric illnesses. Their content, duration and timing relate to their cause and provide useful differential diagnostic information. Hallucinations must be distinguished from delusions and confabulation. A systematic approach to differentiating among hallucinatory syndromes may improve diagnostic accuracy.Dawson, K. A. (2001). A case study of space-time distortion during a total lunar eclipse following street use of LSD. Journal of Psychoactive Drugs, 33(3), 301-305.
Although psychedelics can induce "cosmic" consciousness through severe distortions of time and space perceptions, little attention has been given to examination of this psychopharmacological property. With the hope of providing an impetus to further research in this area, a case of cosmic perception under the influence of LSD is reported which included the apparent movement of consciousness to the lunar surface combined with the experience of remote viewing of the Milky Way galaxy. While the possibility of veridical remote viewing is unlikely, it is speculated that the neurocognitive action of LSD can sensitize the user to focused bright light, associated memories, and creative elaborations during actual eclipse events. Experimenters are urged to adopt precautions to avoid potentially detrimental effects of pharmacologically manipulating the space-time continuum.de Rios, M. D., Grob, C. S., & Baker, J. R. (2002). Hallucinogens and redemption. Journal of Psychoactive Drugs, 34(3), 239-248.
This article examines drug substitution with regard to hallucinogens (ayahuasca, ibogaine, peyote and LSD) set within the concept of redemption. The model examines both religious and secular approaches to the contemporary use of hallucinogens in drug substitution, both by scientists and in religious settings worldwide. The redemptive model posits that the proper use of one psychoactive substance within a spiritual or clinical context helps to free an individual from the adverse effects of their addiction to another substance and thus restores them as functioning members of their community or group. Data is drawn from the U.S., Brazil, Peru, and West Africa. Two principle mechanisms for this are proposed: the psychological mechanism of suggestibility is examined in terms of the individual reaching abstinence goals from addictive substances such as alcohol and opiates. Neurophysiological and neurochemical mechanisms to understand the efficacy of such substitution are highlighted from ongoing research on hallucinogens. Research by two of the authors with the Unaio do Vegetal (UDV) Church in Brazil is examined in terms of the model.Dependence on LSD and other hallucinogenic drugs. (1967). JAMA : The Journal of the American Medical Association, 202(1), 141-144.
Does risperidone exacerbate hallucinogen-persisting perception disorder? (1998). Brown University Psychopharmacology Update, 9(2), 8.
Reports on the findings of a case study published in a 1997 issue of the `Journal of Clinical Psychopharmacology,' about the effectiveness of risperidone in exacerbating hallucinogen-persisting perception disorder. Patient's medical background; Drug abuse history; Contraindications of risperidone.Dumortier, G., Welniarz, B., Sauvebois, C., Medjdoub, H., Friche, H., Siad, N., & Degrassat, K. (2005). Prescription of psychotropic drugs in paediatry: approved indications and therapeutic perspectives. [Prescription des psychotropes en pedopsychiatrie: limites des indications officielles et perspectives therapeutiques] L'Encephale, 31(4 Pt 1), 477-489.
In France, psychotropic drugs may be classified in four categories according to their official data. The first category corresponds to psychotropic drugs with an approved indication available in paediatry. Theyare old agents (e.g. haloperidol, amitriptyline, benzodiazepines...) with the exception of methylphenidate (hyperactivity). The second one corresponds to pharmacological agents approved for some indications obtained with adults but not for a1l (i.e. restricted indication: e.g. sertraline approved in paediatry only for OCD but not for depression, risperidone approved only for the treatment of disruptive behaviors in children with subaverage IQs). For the third category, the psychotropic agent is either contraindicated or unadvised under the age of 15 or 18 years, by lack of data (e.g. most of SSRI or atypical antipsychotic drugs). For the last category, official data available in brief summaries offer no information on paediatric use and consequently their administration does not appear possible. Up to now, no approved use has been delivered to injection route (IM or IV) in France, except for an IM formulation of zuclopenthixol. Prescribing psychotropic drug has to respect good practices including close psychological and somatic monitoring that associates the young patient and his relative (psycho-education program). Particular key-points should be taken into consideration (i.e. pharmacokinetic and physiological specificities, risk of false passage under the age of 6 years with capsules or tablets, presence of alcohol in some oral solution or bitter aroma...). Beside these official data, many studies have been published but must be carefully interpreted according to their level of pertinence. Meta-analysis gather all randomised controlled trials published or not, analyse their specific pertinence and thus provide clinically relevant elements. Randomised controlled trials present clinical interest but key-points in study design must be checked (e.g. number of patients, inclusion and exclusion criteria, length of the study and clinical relevance of clinical scales...). Other studies like open trials or clinical cases do not offersufficient guarantees. Some randomised controlled trials of clinical relevance have been carried out in this population with new pharmacological classes (eg SSRI, atypical antipsychotic drugs) and may lead to extended indications in children and adolescents. According to bibliographic and official data, the main criteria in the prescribing choice may take into consideration the following sis stressing a poor benefit/risk ratio. SSRI may offer better prospects but their use has not been approved in this indication, until now. In OCD, sertraline shows great interest to enhance clinical response and represents the molecule of reference. No drug has been approved for mood disorders in children or adolescent, in France, contrary to USA where lithium can be administered over the age of 12 years. In addition, antiepileptic drugs like carbamazepine or divalproate have conducted to clinical improvement in some studies. Benzodiazepines, hydroxyzine and meprobamate use should be strictly restricted in case of anxiety symptoms but are the only agents approved in this indication despise promising results obtained with SSRI. Transitory insomnia may take advantage of alimemazine prescription (approved use over the age of 36 months). Some typical neuroleptics are indicated in tics or in behaviour disorders associated to autism or related syndromes but present clinical limitations and poor tolerability. Promising clinical trials (randomised or not) have been conducted with new atypical antipsychotic drugs like risperidone. In conclusion, present data available for paediatric use of psychotropic agents emphasizes that safety and effectiveness are not always well established in particular for the treatment of chronic disorders (long term tolerability assessment). Moreover, studies should be carried out to specify factors promoting adherence and quality of life for this young population in order to optimise clinical benefit of drug prescription.Duncan, J. W. (1974). Persisting psychotic states in adolescent drug users. Child Psychiatry and Human Development, 5(1), 51-62.
Dyck, E. (2005). Flashback: psychiatric experimentation with LSD in historical perspective. Canadian Journal of Psychiatry.Revue Canadienne De Psychiatrie, 50(7), 381-388.
In the popular mind, d-lysergic acid diethylamide (LSD) research in psychiatry has long been associated with the CIA-funded experiments conducted by Ewen Cameron at the Allen Memorial Institute in Montreal, Quebec. Despite this reputation, a host of medical researchers in the post World War II era explored LSD for its potential therapeutic value. Some of the most widespread trials in the Western world occurred in Saskatchewan, under the direction of psychiatrists Humphry Osmond (in Weyburn) and Abram Hoffer (in Saskatoon). These medical researchers were first drawn to LSD because of its ability to produce a "model psychosis." Their experiments with the drug that Osmond was to famously describe as a "psychedelic" led them to hypothesize and promote the biochemical nature of schizophrenia. This brief paper examines the early trials in Saskatchewan, drawing on hospital records, interviews with former research subjects, and the private papers of Hoffer and Osmond. It demonstrates that, far from being fringe medical research, these LSD trials represented a fruitful, and indeed encouraging, branch of psychiatric research occurring alongside more famous and successful trials of the first generation of psychopharmacological agents, such as chlropromazine and imipramine. Ultimately, these LSD experiments failed for 2 reasons, one scientific and the other cultural. First, in the 1950s and early 1960s, the scientific parameters of clinical trials shifted to necessitate randomized controlled trials, which the Saskatchewan researchers had failed to construct. Second, as LSD became increasingly associated with student riots, antiwar demonstrations, and the counterculture, governments intervened to criminalize the drug, restricting and then terminating formal medical research into its potential therapeutic effects.Dyer, C. (2002). NHS settles claim of patients treated with LSD. BMJ (Clinical Research Ed.), 324(7336), 501.
Ekbom, K., Waldenlind, E., & Tfelt-Hansen, P. (2009). Cluster headache and aura. Headache, 49(5), 786-787. doi:10.1111/j.1526-4610.2009.01417.x
Ellison, G. D., & Keys, A. S. (1996). Persisting changes in brain glucose uptake following neurotoxic doses of phencyclidine which mirror the acute effects of the drug. Psychopharmacology, 126(3), 271-274.
Phencyclidine (PCP) can induce a model psychosis which has a number of similarities to dementias and schizophrenia. In some cases the psychosis persists for prolonged periods after drug discontinuation. N-Methyl-D-aspartate (NMDA) antagonists such as PCP induce increases in glucose metabolism in a variety of brain structures but most notably in limbic regions such as retrosplenial, piriform, and entorhinal cortex, hippocampus, and olfactory tubercle. When given continuously for several days, these NMDA antagonists induced neural degeneration in these same critical limbic areas. In the present study regional 2-fluorodeoxyglucose (FDG) uptake was measured in rats at both 24 h and 10 days after neurotoxic, 5-day "binge" PCP administration. At 24 h after minipump removal there were persisting and large increases in glucose uptake in many brain regions, with maximal changes in the same limbic structures in which neurotoxicity has been observed. Surprisingly, many of these regions still showed elevated glucose metabolism after 10 days of recovery. These findings suggest an anatomical and neurochemical substrate for the persisting psychosis which can occur following PCP.El-Mallakh, R. S., & Abraham, H. D. (2007). MDMA (Ecstasy). Annals of Clinical Psychiatry : Official Journal of the American Academy of Clinical Psychiatrists, 19(1), 45-52. doi:10.1080/10401230601163592
BACKGROUND: 3,4-Methylenedioxymethamphetamine (MDMA or Ecstasy) is a synthetic amphetamine analogue that is recreationally used to obtain a psychological effect of enhanced affiliative emotional response. Its use in Western countries appears to be increasing, particularly among young individuals. METHODS: Pertinent basic and clinical literature is critically reviewed. RESULTS: A significant body of literature suggests that the patterns of MDMA use differ from traditional drugs of abuse, with relatively uncommon dependence and escalation of dosage. Nonetheless, MDMA is also neurotoxic with significant deleterious effects on serotonergic neurons, memory, and mood. Despite this, there is a dearth of treatment strategies for both acute intoxication and consequences of longer term use. CONCLUSIONS: MDMA is an important drug of abuse that has a wide range of adverse consequences.Espiard, M., Lecardeur, L., Abadie, P., Halbecq, I., & Dollfus, S. (2005). Hallucinogen persisting perception disorder after psilocybin consumption: a case study. European Psychiatry, 20(5-6), 458-460. doi:DOI: 10.1016/j.eurpsy.2005.04.008
Favazza, A. R., & Domino, E. F. (1969). Recurrent LSD experience (flashbacks) triggered by marihuana. University of Michigan Medical Center Journal, 35(4), 214-216.
Fotiou, D. F., Stergiou, V., Tsiptsios, D., Lithari, C., Nakou, M., & Karlovasitou, A. (2009). Cholinergic deficiency in Alzheimer's and Parkinson's disease: Evaluation with pupillometry. International Journal of Psychophysiology, 73(2), 143-149. doi:DOI: 10.1016/j.ijpsycho.2009.01.011
The aim of the study was to evaluate the cholinergic deficiency in Alzheimer's (AD) and Parkinson's disease (PD). For this purpose, pupil size changes and mobility were assessed using a fast-video pupillometer (263 frames/s). Twenty-three (23) patients with probable AD and twenty-two (22) patients with PD (eleven with cognitive impairment and eleven without) entered the study. A full record of the pupil's reaction to light was registered. From this data ten (10) parameters were measured and reported. Comparison of those parameters in both group of subjects followed. Patients with probable AD had abnormal pupillary function compared to healthy ageing. All the Pupil Light Reflex (PLR) variables significantly differed between the two groups (p < 0.005) except the Baseline Pupil Diameter after 2-min dark adaptation (D1) and the Minimum Pupil Diameter (D2). Maximum Constriction Acceleration (ACmax) was the best predictor in classifying a subject as normal or as an AD with a perfect classification ability (AUC = 1, p < 0.001). ACmax and Maximum Constriction Velocity (VCmax) were significantly lower in PD patients without and with coexisting cognitive impairment compared to normal subjects (p < 0.001). Patients with cognitive impairment had significantly lower levels of ACmax, VCmax and amplitude (AMP = D1–D2) than patients with no cognitive deficits. ACmax and secondarily VCmax were the best predictors in classifying a subject as normal or as a PD patient with or without cognitive impairment. Cognitive and memory impairment, which reflects a cholinergic deficit, may be a crucial pathogenetic factor for the decrease in the aforementioned pupillometric parameters. VCmax and ACmax can be considered as the most sensitive indicators of this cholinergic deficiency.Frankel, F. H. (1994). The concept of flashbacks in historical perspective. The International Journal of Clinical and Experimental Hypnosis, 42(4), 321-336.
A computer search of the literature for papers indexed under "flashbacks" produced a list of 70 references, many found in publications on the topics of substance abuse and trauma. Several of these were letters or papers written in languages other than English. In all, the author reviewed 55 papers. Although most of these papers contained comments that addressed the subject matter to some extent as recurrences or reminiscences of past happenings, the variability in the use of the term leaves many unresolved questions regarding the veridicality of the imagery. Nothing in the presentations reviewed by the author clearly demonstrates the unidimensional nature of flashbacks nor any recognizable neurophysiological correlate. The content of a flashback appears to be at least as likely to be the product of imagination as it is of memory.Frecska, E., & Luna, L. E. (2006). The adverse effects of hallucinogens from intramural perspective. Neuropsychopharmacologia Hungarica : A Magyar Pszichofarmakologiai Egyesulet Lapja = Official Journal of the Hungarian Association of Psychopharmacology, 8(4), 189-200.
Very recently, after a long-lasting, worldwide moratorium on research of hallucinogenic agents, a good number of advanced countries have been revising their position, and start to approve testing the physiological and therapeutic effects of hallucinogens in human subjects. The purpose of this article is to review safety information available in the literature on hallucinogen use, and sort out those data from the reported complications of their abuse. Because of prohibitory regulations of the last 35 years, there are difficulties in achieving this kind of evaluation. Our approach has to be broad, and at times retrospective, in contrast to the well-controlled, focused, prospective design of the premarketing trials of legal drugs. The article summarizes the analyses in anticipation of supportive regulatory changes for the use of hallucinogens in well controlled studies and strictly supervised clinical trials. Keywords: adverse effects, ayahuasca, N,N-dimethyltryptamine, hallucinogenic agents, ibogaine, lysergic acid diethylamide, N-methyl-3,4-methylenedioxyamphetamine, psilocybin, therapeutic use.Gaillard, M. C., & Borruat, F. X. (2003). Persisting visual hallucinations and illusions in previously drug-addicted patients. Klinische Monatsblatter Fur Augenheilkunde, 220(3), 176-178. doi:10.1055/s-2003-38173
BACKGROUND: Tetrahydrocannabinol (cannabis) and lysergic acid diethylamide (LSD) are psychomimetic agents that induce impairment of sensory perception. Illusions and hallucinations are mostly visual. Most frequently the visual phenomena occur in conjunction with drug abuse. PATIENTS AND METHODS: Three previously drug-addicted patients were examined for either persisting or spontaneously recurrent visual phenomena. Two patients complained of persisting visual illusions (vibrations, dyskinetopsia and impaired depth perception) during more than 12 months after an excessive use of cannabis. The third patient was a multiple drug abuser (LSD for 6 years) and complained of visual hallucinations and palinopsia following heavy ethanol intake, 20 years after stopping the use of any drug. RESULTS: Results from neuro-ophthalmic and neurological examinations were normal for the first two patients. The third patient presented abnormal visual fields with preserved visual acuity; electroencephalography was abnormal, suggesting an underlying toxic encephalopathy. CONCLUSIONS: Persistent visual illusions or hallucinations can occur during several months after an intake of cannabis. Flash-back phenomena are frequent amongst LSD abusers. They rarely occur at long times after the last intake (20 years in the present case); when they do so, precipitating factors are often present (ethanol, medication, anesthesia). Such phenomena reflect the cortical dysfunctions that can be induced by illegal substances.Giorgi, F. S., Lazzeri, G., Natale, G., Iudice, A., Ruggieri, S., Paparelli, A., Murri, L., & Fornai, F. (2006). MDMA and seizures: a dangerous liaison? Annals of the New York Academy of Sciences, 1074, 357-364. doi:10.1196/annals.1369.035
In the past decades, there was a massive increase in the abuse of methylenedioxymethamphetamine (MDMA) in the Western countries. Seizure onset after MDMA is considered to be related mainly to its acute systemic effects (e.g., hyponatremia and hyperthermia). However, additional mechanisms might concur to it as well. Experiments aimed at disclosing the basis for such an acute effect have the advantage of profiting of controlled conditions and the "pure" compounds, as opposed to the limits of clinical data which are biased by several confounding factors. Amphetamines exert profound effect on different monoaminergic systems, which might participate to lowering of seizure threshold. Chronic effects of MDMA abuse on seizure threshold have not been explored in detail so far. Recent data showed that in mice receiving small, repeated doses of MDMA, a persisting pro-convulsant effect toward limbic seizures and metabolic hyperexcitability can be observed. In the present article, we reviewed these studies and we report our preliminary experimental data documenting the lack of mossy fiber sprouting at short time intervals following MDMA, when seizure susceptibility is already present.Gouzoulis-Mayfrank, E., Daumann, J., & Sass, H. (2002). Chronic neurotoxic damage in ecstasy (MDMA) users. Review of the current state of research. [Neurotoxische Langzeitschaden bei Ecstasy (MDMA)-Konsumenten. Uberblick uber den aktuellen Wissensstand] Der Nervenarzt, 73(5), 405-421.
The popular dance drug ecstasy (3,4-methylenedioxymethamphetamine, or MDMA, and some analogues) causes selective and persistent neurotoxic damage of the central serotonergic system in laboratory animals. Serotonin plays a role in numerous functional systems in the CNS. Consequently, various abnormalities including psychiatric, vegetative, neuroendocrine, and cognitive disorders might be expected in humans following damage of the central serotonergic system. In recent years, the questions of possible functional disorders following ecstasy-induced neurotoxicity were addressed in several cross-sectional studies with drug users. In this review we summarize and evaluate the quality of design of these studies. Despite large methodological problems, evidence accumulates in favor of persisting brain damage in ecstasy users resulting in subtle cognitive deterioration. Findings of relatively low memory performance associated with heavy ecstasy use are highly consistent across different studies and user populations. In addition, low performance in tests of higher executive function were reported in some but not all studies. The important questions about progression, persistence, or reversibility of damage after long periods of abstinence have to be addressed in future studies with longitudinal design.Gresch, P. J., Smith, R. L., Barrett, R. J., & Sanders-Bush, E. (2005). Behavioral tolerance to lysergic acid diethylamide is associated with reduced serotonin-2A receptor signaling in rat cortex. Neuropsychopharmacology : Official Publication of the American College of Neuropsychopharmacology, 30(9), 1693-1702. doi:10.1038/sj.npp.1300711
Tolerance is defined as a decrease in responsiveness to a drug after repeated administration. Tolerance to the behavioral effects of hallucinogens occurs in humans and animals. In this study, we used drug discrimination to establish a behavioral model of lysergic acid diethylamide (LSD) tolerance and examined whether tolerance to the stimulus properties of LSD is related to altered serotonin receptor signaling. Rats were trained to discriminate 60 microg/kg LSD from saline in a two-lever drug discrimination paradigm. Two groups of animals were assigned to either chronic saline treatment or chronic LSD treatment. For chronic treatment, rats from each group were injected once per day with either 130 microg/kg LSD or saline for 5 days. Rats were tested for their ability to discriminate either saline or 60 microg/kg LSD, 24 h after the last chronic injection. Rats receiving chronic LSD showed a 44% reduction in LSD lever selection, while rats receiving chronic vehicle showed no change in percent choice on the LSD lever. In another group of rats receiving the identical chronic LSD treatment, LSD-stimulated [35S]GTPgammaS binding, an index of G-protein coupling, was measured in the rat brain by autoradiography. After chronic LSD, a significant reduction in LSD-stimulated [35S]GTPgammaS binding was observed in the medial prefrontal cortex and anterior cingulate cortex. Furthermore, chronic LSD produced a significant reduction in 2,5-dimethoxy-4-iodoamphetamine-stimulated [35S]GTPgammaS binding in medial prefrontal cortex and anterior cingulate cortex, which was blocked by MDL 100907, a selective 5-HT2A receptor antagonist, but not SB206553, a 5-HT2C receptor antagonist, indicating a reduction in 5-HT2A receptor signaling. 125I-LSD binding to 5-HT2A receptors was reduced in cortical regions, demonstrating a reduction in 5-HT2A receptor density. Taken together, these results indicate that adaptive changes in LSD-stimulated serotonin receptor signaling may mediate tolerance to the discriminative stimulus effects of LSD.Griffiths, R. R., Richards, W. A., McCann, U., & Jesse, R. (2006). Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology, 187(3), 268-83; discussion 284-92. doi:10.1007/s00213-006-0457-5
RATIONALE: Although psilocybin has been used for centuries for religious purposes, little is known scientifically about its acute and persisting effects. OBJECTIVES: This double-blind study evaluated the acute and longer-term psychological effects of a high dose of psilocybin relative to a comparison compound administered under comfortable, supportive conditions. MATERIALS AND METHODS: The participants were hallucinogen-naive adults reporting regular participation in religious or spiritual activities. Two or three sessions were conducted at 2-month intervals. Thirty volunteers received orally administered psilocybin (30 mg/70 kg) and methylphenidate hydrochloride (40 mg/70 kg) in counterbalanced order. To obscure the study design, six additional volunteers received methylphenidate in the first two sessions and unblinded psilocybin in a third session. The 8-h sessions were conducted individually. Volunteers were encouraged to close their eyes and direct their attention inward. Study monitors rated volunteers' behavior during sessions. Volunteers completed questionnaires assessing drug effects and mystical experience immediately after and 2 months after sessions. Community observers rated changes in the volunteer's attitudes and behavior. RESULTS: Psilocybin produced a range of acute perceptual changes, subjective experiences, and labile moods including anxiety. Psilocybin also increased measures of mystical experience. At 2 months, the volunteers rated the psilocybin experience as having substantial personal meaning and spiritual significance and attributed to the experience sustained positive changes in attitudes and behavior consistent with changes rated by community observers. CONCLUSIONS: When administered under supportive conditions, psilocybin occasioned experiences similar to spontaneously occurring mystical experiences. The ability to occasion such experiences prospectively will allow rigorous scientific investigations of their causes and consequences.Halpern, J. H., & Pope, H. G.,Jr. (2003). Hallucinogen persisting perception disorder: what do we know after 50 years? Drug and Alcohol Dependence, 69(2), 109-119.
'Flashbacks' following use of hallucinogenic drugs have been reported for decades; they are recognized in DSM-IV as 'Hallucinogen Persisting Perception Disorder (Flashbacks)', or HPPD. We located and analyzed 20 quantitative studies between 1955 and 2001 examining this phenomenon. However, many of these studies were performed before operational criteria for HPPD were published in DSM-III-R, so they are difficult to interpret in the light of current diagnostic criteria. Overall, current knowledge of HPPD remains very limited. In particular (1) the term 'flashbacks' is defined in so many ways that it is essentially valueless; (2) most studies provide too little information to judge how many cases could meet DSM-IV criteria for HPPD; and consequently (3) information about risk factors for HPPD, possible etiologic mechanisms, and potential treatment modalities must be interpreted with great caution. At present, HPPD appears to be a genuine but uncommon disorder, sometimes persisting for months or years after hallucinogen use and causing substantial morbidity. It is reported most commonly after illicit LSD use, but less commonly with LSD administered in research or treatment settings, or with use of other types of hallucinogens. There are case reports, but no randomized controlled trials, of successful treatment with neuroleptics, anticonvulsants, benzodiazepines, and clonidine. Although it may be difficult to collect large samples of HPPD cases, further studies are critically needed to augment the meager data presently available regarding the prevalence, etiology, and treatment of HPPD.Hasse, H. E., & Waldmann, H. (1971). "Flashback": spontaneous psychotic episodes in adolescence resulting from psychedelic drug use. ["Flashback": Spontane psychotische Episoden als Folgeerscheinung des Phantasticagebrauchs Jugendlicher] Archiv Fur Psychiatrie Und Nervenkrankheiten, 214(4), 399-439.
Haynes, J. (2009). Decoding visual consciousness from human brain signals. Trends in Cognitive Sciences, 13(5), 194-202. doi:DOI: 10.1016/j.tics.2009.02.004
Heinrich, S. P., Mell, D., & Bach, M. (2009). Frequency-domain analysis of fast oddball responses to visual stimuli: A feasibility study. International Journal of Psychophysiology, 73(3), 287-293. doi:DOI: 10.1016/j.ijpsycho.2009.04.011
Event-related potential responses to oddball stimuli, including the P300 component, have been proposed as a diagnostic tool for discerning psychiatric or higher-level neural disorders from malingering, for instance in cases of unexplained visual loss. For clinical use, short recording durations and easy statistical assessment are highly desirable. With this aim, we investigated the feasibility of recording oddball responses in a fast steady-state regime. We used gratings with two possible orientations in a rapid oddball paradigm with an inter-stimulus interval of 214 ms. Six consecutive presentations of one stimulus type (frequent) were followed by a single presentation of the other (infrequent) stimulus type. Subjects were attending to the rare stimulus type. The electroencephalographic recordings were analyzed in the frequency domain. All subjects produced significant harmonic responses related to the processing of the rare stimulus, demonstrating the feasibility of the technique, with the potential of reducing recording times substantially compared to conventional slow stimulation. We furthermore found that the regularity of the occurrence of infrequent stimuli, which is necessary for frequency-domain analysis, does not per se reduce the P300 responses, as would have been expected in the framework of some hypotheses regarding the role of the P300.Hermle, L., Kovar, K. A., Hewer, W., & Ruchsow, M. (2008). Hallucinogen-induced psychological disorders. [Halluzinogen-induzierte psychische Storungen] Fortschritte Der Neurologie-Psychiatrie, 76(6), 334-342. doi:10.1055/s-2008-1038191
OBJECTIVE: The purpose of this article is to provide an overview of the current research on hallucinogen induced psychiatric disorders. In addition to LSD and psilocybin hallucinogens of biologic origin are increasingly used by adolescents and young adults. METHODS: Relevant literature and related articles were identified by means of a computerized MEDLINE search including the years 1997 - 2007. As keywords "hallucinogen induced psychosis", "hallucinogen induced flashback", "hallucinogen persisting perception disorder (HPPD)" were used. Finally, 64 journal articles and books out of 103 were included in the review. RESULTS: Acute psychotic syndromes in adolescents are rarely due to intoxications with hallucinogenic drugs. However, clinical relevance of flashback phenomena as post-hallucinogenic psychiatric disorder has to be disputed. Because of the high popularity of biogenic hallucinogens and LSD knowledge of intoxications and resulting psychiatric disorders as well as medical complications and therapeutical approaches are clinically important. Especially intoxications with drugs of herbal origin like tropanalcaloids play an important role in emergency situations.Holsten, F. (1974). Flashbacks--late reactions after LSD and cannabis use among 78 drug addicts. ["Flashbacks"--senreaksjoner etter bruk av LSD og cannabis hos 78 stoffbrukere] Tidsskrift for Den Norske Laegeforening : Tidsskrift for Praktisk Medicin, Ny Raekke, 94(30), 2070-2077.
Holsten, F. (1976). Flashbacks: a personal follow-up. Archiv Fur Psychiatrie Und Nervenkrankheiten, 222(4), 293-304.
During the period 1971-1973, it was found that 53 out of 91 young drug abusers in a psychiatric hospital had experienced flashbacks. This applied to as many as 50 out of the 65 patients who had used LSD, but also to abusers of organic solvents and cannabis. As many as 38% of the patients were found to be severely incapacitated by their flashbacks. On a personal follow-up 1 1/2-4 years after the first therapeutic contact, 35 patients were still troubled by flashbacks. On the whole reactions were less intense than at the time of the first contact. No relation between the flashbacks and protracted psychotic development could be established. The overall clinical and social course was worse for patients with flashbacks than for the rest of the population. Patients still bothered by flashbacks used drugs and alcohol as sedatives to a greater extent than the rest.Horowitz, M. J. (1969). Flashbacks: recurrent intrusive images after the use of LSD. The American Journal of Psychiatry, 126(4), 565-569.
Ikeda, A., Sekiguchi, K., Fujita, K., Yamadera, H., & Koga, Y. (2005). 5-methoxy-N,N-diisopropyltryptamine-induced flashbacks. The American Journal of Psychiatry, 162(4), 815. doi:10.1176/appi.ajp.162.4.815
Johnson, M., Richards, W., & Griffiths, R. (2008). Human hallucinogen research: guidelines for safety. Journal of Psychopharmacology (Oxford, England), 22(6), 603-620. doi:10.1177/0269881108093587
There has recently been a renewal of human research with classical hallucinogens (psychedelics). This paper first briefly discusses the unique history of human hallucinogen research, and then reviews the risks of hallucinogen administration and safeguards for minimizing these risks. Although hallucinogens are relatively safe physiologically and are not considered drugs of dependence, their administration involves unique psychological risks. The most likely risk is overwhelming distress during drug action ('bad trip'), which could lead to potentially dangerous behaviour such as leaving the study site. Less common are prolonged psychoses triggered by hallucinogens. Safeguards against these risks include the exclusion of volunteers with personal or family history of psychotic disorders or other severe psychiatric disorders, establishing trust and rapport between session monitors and volunteer before the session, careful volunteer preparation, a safe physical session environment and interpersonal support from at least two study monitors during the session. Investigators should probe for the relatively rare hallucinogen persisting perception disorder in follow-up contact. Persisting adverse reactions are rare when research is conducted along these guidelines. Incautious research may jeopardize participant safety and future research. However, carefully conducted research may inform the treatment of psychiatric disorders, and may lead to advances in basic science.Juve, J. L. (1972). Bad drug trips and flashbacks. Child Welfare, 51(1), 41-50.
Kawasaki, A., & Purvin, V. (1996). Persistent palinopsia following ingestion of lysergic acid diethylamide (LSD). Archives of Ophthalmology, 114(1), 47-50.
OBJECTIVE: To identify a distinctive chronic visual complication of lysergic acid diethylamide (LSD) use. DESIGN: Description of the clinical findings in three patients with this disorder. SETTING: A neuro-ophthalmology referral center. RESULTS: All three patients experienced prolonged afterimages (palinopsia) during LSD intoxication and have continued to be symptomatic up to 3 years after they ceased to ingest the drug. Results of neuro-ophthalmologic and neurologic examinations and neuroimaging and electrophysiologic studies were normal. CONCLUSIONS: We have described three patients in whom persistent palinopsia developed following ingestion of LSD. Clinicians should inquire about past LSD use in all patients who initially have seemingly spontaneous, isolated palinopsia. Recognition of this distinctive clinical syndrome associated with LSD use might avoid unnecessary anxiety and excessive diagnostic tests for patients with this disorder.King, W.,Jr, & Ellison, G. (1989). Long-lasting alterations in behavior and brain neurochemistry following continuous low-level LSD administration. Pharmacology, Biochemistry, and Behavior, 33(1), 69-73.
Groups of rats were administered either 80 micrograms LSD-25 continuously over seven days using subcutaneous minipumps, or were given the same total amount of drug in seven daily injections, or were administered vehicle. When tested long after cessation of drug administration, persisting alterations in behavior and brain were found in the continuous LSD groups. In social open-field tests, this consisted of decreased social distance between animals; this effect increased upon repeated testing. In uptake of labeled ligands, this was reflected predominantly by decreased 3H-LSD binding in several limbic regions. LSD appears to have especially persisting neurotoxic effects when administered in a continuous, low-level fashion.Kolmel, H. W. (1985). Complex visual hallucinations in the hemianopic field Journal of Neurology, Neurosurgery, and Psychiatry, 48(1), 29-38.
From 120 patients with an homonymous hemianopia 16 experienced complex visual hallucinations in the hemianopic field. The brain lesion was located in the occipital lobe, though damage was not limited to this area. Complex hallucinations appeared after a latent period. They were weak in colour and stereotypical in appearance, which allowed differentiation from visual hallucinations of other causes. Different behaviour after saccadic eye movement differentiated between complex visual hallucinations in the hemianopic field and visual auras of an epileptic origin.Lauterbach, E. C., Abdelhamid, A., & Annandale, J. B. (2000). Posthallucinogen-like visual illusions (palinopsia) with risperidone in a patient without previous hallucinogen exposure: possible relation to serotonin 5HT2a receptor blockade. Pharmacopsychiatry, 33(1), 38-41.
BACKGROUND: Previous reports document visual illusions resembling hallucinogen persisting perception disorder (HPPD) after risperidone treatment in patients with histories of previous LSD exposure. METHODS: We report a case with visual disturbances resembling HPPD after each of three consecutive risperidone dose increases. RESULTS: Contrasting with previous reports, our patient lacked any history of substance abuse, particularly hallucinogen exposure. She lacked neurologic or other contributory illnesses. Illusions generally remitted within 48 hours each time. Coadministration of trazodone and clonazepam may have contributed to these phenomena, although clonazepam has been used to treat this condition. She had been unusually sensitive to the side-effects of many psychotropics. CONCLUSIONS: This case is unique due to the absence of substance abuse. This and another report note heightened sensitivity to medication side-effects. Visual phenomena resembling HPPD evidently can occur with risperidone and, possibly, other atypical antipsychotics and certain antidepressants regardless of previous hallucinogen use. Several lines of evidence implicate reduced 5HT2a serotonin receptor stimulation rather than increased 5HT2c stimulation.Leikin, J. B., Krantz, A. J., Zell-Kanter, M., Barkin, R. L., & Hryhorczuk, D. O. (1989). Clinical features and management of intoxication due to hallucinogenic drugs. Medical Toxicology and Adverse Drug Experience, 4(5), 324-350.
Hallucinogenic drugs are unique in that they produce the desired hallucinogenic effects at what are considered non-toxic doses. The hallucinogenic drugs can be categorised into 4 basic groups: indole alkaloid derivatives, piperidine derivatives, phenylethylamines and the cannabinols. The drugs reviewed include lysergic acid diethylamide (LSD), phencyclidine (PCP), cocaine, amphetamines, opiates, marijuana, psilocybin, mescaline, and 'designer drugs.' Particularly noteworthy is that each hallucinogen produces characteristic behavioural effects which are related to its serotonergic, dopaminergic or adrenergic activity. Cocaine produces simple hallucinations, PCP can produce complex hallucinations analogous to a paranoid psychosis, while LSD produces a combination of hallucinations, pseudohallucinations and illusions. Dose relationships with changes in the quality of the hallucinatory experience have been described with amphetamines and, to some extent, LSD. Flashbacks have been described with LSD and alcohol. Management of the intoxicated patient is dependent on the specific behavioural manifestation elicited by the drug. The principles involve differentiating the patient's symptoms from organic (medical or toxicological) and psychiatric aetiologies and identifying the symptom complex associated with the particular drug. Panic reactions may require treatment with a benzodiazepine or haloperidol. Patients with LSD psychosis may require an antipsychotic. Patients exhibiting prolonged drug-induced psychosis may require a variety of treatments including ECT, lithium and l-5-hydroxytryptophan.Lerner, A. G., Finkel, B., Oyffe, I., Merenzon, I., & Sigal, M. (1998). Clonidine treatment for hallucinogen persisting perception disorder. The American Journal of Psychiatry, 155(10), 1460.
Lerner, A. G., Gelkopf, M., Oyffe, I., Finkel, B., Katz, S., Sigal, M., & Weizman, A. (2000). LSD-induced hallucinogen persisting perception disorder treatment with clonidine: an open pilot study. International Clinical Psychopharmacology, 15(1), 35-37.
A pilot open study was conducted in order to evaluate the efficacy of clonidine in the treatment of LSD-induced hallucinogen persisting perception disorder (HPPD). Eight patients fulfilled entrance criteria. All complained of HPPD for at least 3 months and were drug free at least 3 months. They received fixed low doses of clonidine, 0.025 mg, three times a day for 2 months. They were evaluated by the Clinical Global Impression Scale (CGI) and a self-report scale on the severity of symptoms (graded 0-5). Patients scored an average of 5.25 (SD = 0.46) on the CGI and 4 on the self-report scale at baseline, indicating marked psychopathology. One patient dropped out at week 3 and a second patient dropped out at week 5. Of the six patients remaining at the end of 2 months, the average CGI score was 2.5 (SD = 0.55) and the self-report scale score was 2, indicating mild symptomatology. LSD-related flashbacks associated with excessive sympathetic nervous activity may be alleviated with clonidine in some patients.Lerner, A. G., Gelkopf, M., Skladman, I., Oyffe, I., Finkel, B., Sigal, M., & Weizman, A. (2002). Flashback and Hallucinogen Persisting Perception Disorder: clinical aspects and pharmacological treatment approach. The Israel Journal of Psychiatry and Related Sciences, 39(2), 92-99.
One unique characteristic of lysergic acid diethylamide (LSD) and LSD-like substances is the recurrence of some of the symptoms which appeared during the intoxication after the immediate effect of the hallucinogen has worn off. This recurring syndrome, mainly visual, has not been clearly understood, appreciated or distinguished from other clinical entities by clinicians. The terms Flashback and Hallucinogen Persisting Perception Disorder (HPPD) are used interchangeably in the professional literature. Flashback is a usually short-term, non-distressing, spontaneous, recurrent, reversible and benign condition accompanied by a pleasant affect. In contrast, HPPD is a generally long-term, distressing, spontaneous, recurrent, pervasive, either slowly reversible or irreversible, non-benign condition accompanied by an unpleasant dysphoric affect. Flashback and HPPD appear to be part of a vast and broad spectrum of non-psychopathological and psychopathological states reported by hallucinogen users. Pharmacological agents such as clonidine, perphenazine and clonazepan have been shown to ameliorate this syndrome in some of the individuals seeking treatment.Lerner, A. G., Gelkopf, M., Skladman, I., Rudinski, D., Nachshon, H., & Bleich, A. (2003). Clonazepam treatment of lysergic acid diethylamide-induced hallucinogen persisting perception disorder with anxiety features. International Clinical Psychopharmacology, 18(2), 101-105. doi:10.1097/01.yic.0000053665.88477.46
An unique and intriguing characteristic of lysergic acid diethylamide (LSD) and LSD-like substances is the recurrence of some of the symptoms which appear during the intoxication, in the absence of recent intake of hallucinogens. Hallucinogen persisting perception disorder (HPPD) is a condition in which the re-experiencing of one or more perceptual symptoms causes significant distress or impairment in social, occupational or other important areas of functioning and may be extremely debilitating. Benzodiazepines are one of the recommended agents for the treatment of HPPD but it is unclear which of them may be more helpful. The goal of our investigation was to assess the efficacy of clonazepam in the treatment of LSD-induced HPPD. Sixteen patients fulfilled entrance criteria. All complained of HPPD with anxiety features for at least 3 months and were drug free at least 3 months. They received clonazepam 2 mg/day for 2 months. Follow-up was continued for 6 months. They were weekly evaluated during the 2 months of clonazepam administration and monthly during the follow-up period using the Clinical Global Impression Scale, a Self-report Scale and Hamilton Anxiety Rating Scale. Patients reported a significant relief and the presence of only mild symptomatology during the clonazepam administration. This improvement was clearly sustained and persisted during a 6-month follow-up period. This study suggests that high potency benzodiazepines like clonazepam, which has serotonergic properties, may be more effective than low-potency benzodiazepines in the treatment of some patients with LSD-induced HPPD.Lerner, A. G., Oyefe, I., Isaacs, G., & Sigal, M. (1997). Naltrexone treatment of hallucinogen persisting perception disorder. The American Journal of Psychiatry, 154(3), 437.
Lerner, A. G., Shufman, E., Kodesh, A., Kretzmer, G., & Sigal, M. (2002). LSD-induced Hallucinogen Persisting Perception Disorder with depressive features treated with reboxetine: case report. The Israel Journal of Psychiatry and Related Sciences, 39(2), 100-103.
We would like to present the case of a patient who had a prior history of cannabis, ecstasy (MDMA) and LSD abuse and who developed both Hallucinogen Persisting Perception Disorder (HPPD) and a major depressive episode. Following two unsuccessful SSRIs trials, reboxetine was prescribed. During a six-month follow-up period on reboxetine 6 mg./day, no exacerbation of the visual disturbance or recurrence of the depressive features were reported. Reboxetine may have an alpha 2 adrenoreceptor modulating effect on both noradrenaline and serotonin release, thus reboxetine's alpha 2 adrenoreceptor modulating effect on noradrenaline release may affect sympathetic activity and be involved in the recovery process.Lerner, A. G., Skladman, I., Kodesh, A., Sigal, M., & Shufman, E. (2001). LSD-induced Hallucinogen Persisting Perception Disorder treated with clonazepam: two case reports. The Israel Journal of Psychiatry and Related Sciences, 38(2), 133-136.
Benzodiazepines are recommended for the treatment of Hallucinogen Persisting Perception Disorder (HPPD), although it is unclear which may be more helpful. Two out-patients with LSD-induced HPPD were successfully treated with clonazepam. They had not responded to low potency benzodiazepines or low doses of classic antipsychotics. After clonazepam discontinuation they reported a marked improvement and only mild symptomatology which persisted during a six month follow-up period. High potency benzodiazepines like clonazepam, which has serotonergic properties, may be superior to low-potency benzodiazepines in the treatment of some patients with LSD-induced HPPD.Linszen, D., & van Amelsvoort, T. (2007). Cannabis and psychosis: an update on course and biological plausible mechanisms. Current Opinion in Psychiatry, 20(2), 116-120. doi:10.1097/YCO.0b013e32803577fb
PURPOSE OF REVIEW: Cannabis use is the most commonly abused illicit substance. Its relation with psychosis remains a topic of debate. Epidemiological studies suggest that cannabis is a component cause accounting for approximately 10% of cases. An increasing number of studies have been published on neurobiological effects of cannabis and vulnerability of psychosis. RECENT FINDINGS: Acute cannabis administration can induce memory impairments, sometimes persisting months following abstinence. There is no evidence that residual effects on cognition remain after years of abstinence. The scarce literature on neuro-imaging mainly done in nonpsychotic populations, show little evidence that cannabis has effects on brain anatomy. Acute effects of cannabis include increases of cerebral blood flow, whereas long-term effects of cannabis include attenuation of cerebral blood flow. In animals Delta9-tetrahydrocannabinol enhances dopaminergic neurotransmission in brain regions known to be implicated in psychosis. Studies in humans show that genetic vulnerability may add to increased risk of developing psychosis and cognitive impairments following cannabis consumption. Delta9-tetrahydrocannabinol induces psychotic like states and memory impairments in healthy volunteers. SUMMARY: Simultaneously with increasing understanding of neurobiological cannabis effects, there is a lack of studies in people with psychosis. There are plausible mechanisms that might explain the psychotogenic effects of cannabis.Madden, J. S. (1994). LSD and post-hallucinogen perceptual disorder. Addiction (Abingdon, England), 89(6), 762-763.
Markel, H., Lee, A., Holmes, R. D., & Domino, E. F. (1994). LSD flashback syndrome exacerbated by selective serotonin reuptake inhibitor antidepressants in adolescents. The Journal of Pediatrics, 125(5 Pt 1), 817-819.
Two adolescents with a long history of abuse of lysergic acid diethylamide (LSD) and symptoms consistent with major depressive disorder, on initiation of antidepressant therapy with selective serotonin reuptake inhibitor agents, had the new onset or worsening of LSD flashback syndrome. The similarity in neuroreceptor physiology for both LSD and serotonin suggests that the LSD flashback syndrome may be induced by these drugs in patients with a history of LSD abuse.Matefy, R. E., & Krall, R. G. (1974). An initial investigation of the psychedelic drug flashback phenomena. Journal of Consulting and Clinical Psychology, 42(6), 854-860.
Mathias, S., Lubman, D. I., & Hides, L. (2008). Substance-induced psychosis: a diagnostic conundrum. The Journal of Clinical Psychiatry, 69(3), 358-367.
OBJECTIVE: To critically examine the DSM-IV-TR criteria for substance-induced psychotic disorder (SIPD). DATA SOURCES: Leading electronic databases (such as MEDLINE, PubMed) were searched for the years 1992 through 2007, using combinations of the following key search terms: substance abuse/dependence, alcohol, marijuana, cannabis, methamphetamine, crack, cocaine, amphetamine, ecstasy, ketamine, phencyclidine, LSD, mental health, drug-induced psychosis, substance-induced psychosis, psychosis, and schizophrenia. References identified from bibliographies of pertinent articles and books in the field were also collected and reviewed. DATA EXTRACTION: Only research studies or case reports/series that presented data on populations diagnosed with SIPD by using clinical or structured diagnostic interviews and that were published in English were used to assess the validity of the current SIPD criteria. DATA SYNTHESIS: We identified 49 articles that presented clinical data on SIPD. Almost half of these publications were case reports, with 18 articles specifically focusing on delineating the clinical characteristics or outcomes of individuals diagnosed with SIPD. While several large studies have recently been conducted to assess the stability of SIPD, there is a dearth of research that rigorously examines the validity of DSM-IV diagnostic criteria across substances. CONCLUSIONS: There remains a striking paucity of information on the outcome, treatment, and best practice for substance-associated psychotic episodes. Further work is clearly required before the advent of DSM-V. We propose an alternative, broader classification that better reflects the current evidence base, inferring association rather than causation.Mauricio Sierra, M. D., Ph.D. (2009). Depersonalization: A New Look at a Neglected Syndrome. New York: Cambridge University Press.
Depersonalization is a dissociative disorder, causing alteration in the perception or experience of the self and a detachment from reality. This is a fascinating and clinically relevant phenomenon neglected within psychiatry. Far from being a rare condition, it can be as prevalent as schizophrenia or bipolar disorder and frequently occurs in association with other neuropsychiatric conditions. This is an up-to-date review of depersonalization, dealing with the subject from a wide range of perspectives and covering historical, conceptual, clinical, trans-cultural, pharmacological and neurobiological factors. It discusses recent neuroimaging studies providing fresh insights into the condition and opening up new opportunities to manage the symptoms with pharmacologic and psychotherapeutic interventions. As a reference book on depersonalization it represents a timely and highly relevant contribution to fill an unjustified gap in the psychiatric literature. It will be relevant to psychiatrists and clinical psychologists, as well as primary care practitioners, neurologists and psychiatric nurses.McCambridge, J., Winstock, A., Hunt, N., & Mitcheson, L. (2007). 5-Year trends in use of hallucinogens and other adjunct drugs among UK dance drug users. European Addiction Research, 13(1), 57-64. doi:10.1159/000095816
AIMS: To describe and assess trends in the use of hallucinogens and other adjunct drugs over a 5-year period. DESIGN: Repeated-measures cross-sectional survey. SETTING AND PARTICIPANTS: Annual magazine-based survey targeting people who use drugs in dance contexts. MEASUREMENTS: Lifetime use prevalence (ever used); age of first use; current use prevalence (any use within the last month), and extent of use within the last month (number of days used) for LSD, psilocybin, ketamine, GHB and nitrates. FINDINGS: Prevalence increases for psilocybin, ketamine, GHB and nitrates use have been detected, with a sharp recent rise in current psilocybin use in 2002-2003 contrasting with more gradual and comprehensive evidence of increased ketamine use throughout the period 1999-2003. The declining prevalence of LSD use in general population surveys is replicated in this sentinel population study. CONCLUSIONS: The rise in prevalence of hallucinogen and other adjunct drugs identified among dance drug users may be mirrored by wider prevalence increases among young people with a consequent need to study these trends carefully and to develop effective interventions, where required.McGee, R. (1984). Flashbacks and memory phenomena. A comment on "Flashback phenomena--clinical and diagnostic dilemmas". The Journal of Nervous and Mental Disease, 172(5), 273-278.
Alarcon, Dickinson, and Dohn (J. Nerv. Ment. Dis., 170: 217-223, 1982) recently reviewed the phenomenon of memory flashback following use of hallucinogenic drugs. They point out that while there are a considerable number of explanations concerning the flashback mechanism, little is known about the real causes. This paper examines flashback following drug ingestion in the light of other memory phenomena concerned with "cued retrieval" effects. Such phenomena may include dream recall, delayed post-traumatic stress, mood influence on memory, and drug effects on memory. Rather than view flashbacks as "pathological" in some sense, it may be better to view them as instances of normal memory processes, which may, nevertheless, be accompanied by emotional distress. Such a view relates flashbacks to a wider memory literature, and also makes them amenable to investigation using research designs derived from that literature.Morehead, D. B. (1997). Exacerbation of hallucinogen-persisting perception disorder with risperidone. Journal of Clinical Psychopharmacology, 17(4), 327-328.
Moskowitz, D. (1971). Use of haloperidol to reduce LSD flashbacks. Military Medicine, 136(9), 754-756.
Mula, M., Pini, S., Calugi, S., Preve, M., Masini, M., Giovannini, I., Conversano, C., Rucci, P., & Cassano, G. B. (2008). Validity and reliability of the Structured Clinical Interview for Depersonalization-Derealization Spectrum (SCI-DER) Neuropsychiatric Disease and Treatment, 4(5), 977-986.
THIS STUDY EVALUATES THE VALIDITY AND RELIABILITY OF A NEW INSTRUMENT DEVELOPED TO ASSESS SYMPTOMS OF DEPERSONALIZATION: the Structured Clinical Interview for the Depersonalization-Derealization Spectrum (SCI-DER). The instrument is based on a spectrum model that emphasizes soft-signs, sub-threshold syndromes as well as clinical and subsyndromal manifestations. Items of the interview include, in addition to DSM-IV criteria for depersonalization, a number of features derived from clinical experience and from a review of phenomenological descriptions. Study participants included 258 consecutive patients with mood and anxiety disorders, 16.7% bipolar I disorder, 18.6% bipolar II disorder, 32.9% major depression, 22.1% panic disorder, 4.7% obsessive compulsive disorder, and 1.5% generalized anxiety disorder; 2.7% patients were also diagnosed with depersonalization disorder. A comparison group of 42 unselected controls was enrolled at the same site. The SCI-DER showed excellent reliability and good concurrent validity with the Dissociative Experiences Scale. It significantly discriminated subjects with any diagnosis of mood and anxiety disorders from controls and subjects with depersonalization disorder from controls. The hypothesized structure of the instrument was confirmed empirically.Naditch, M. P., & Fenwick, S. (1977). LSD flashbacks and ego functioning. Journal of Abnormal Psychology, 86(4), 352-359.
Neisser, U. (1967). Cognitive psychology. New York,: Appleton-Century-Crofts.
Niveau, G. (2002). Cannabis-related flash-back, a medico-legal case. [Flash-back cannabique, un cas medico-legal] L'Encephale, 28(1), 77-79.
Cannabis is a psychoactive drug more and more widely consumed in industrialized countries and in the world. Amongst the numerous effects it can induce, flashback phenomena have been scientifically recognized only since the 70's. This case regards a young man who offended a friend without any objective reason. The report of the forensic psychiatrist demonstrated that the offense was committed under the influence of a cannabis flashback. The last time the offender had consummed cannabis, probably from Netherland, was two weeks before the acts. A plasmatic detection was realized and showed a level at 6 ng/mL, thirty minutes after the beginning of the flashback. This case confirms the clinical entity of cannabis flashback and gives an exceptional indication on THC blood concentration at the time of the relapse. But the pharmacokinetics of the phenomenon are largely unknown and long term studies concerning the metabolism, not only of THC but also of its metabolites, are needful. On the forensic standpoint, the possible participation of flashback phenomena must not be neglected when grounds of unexplained accidents or crimes are searched.Niwa, K., & Tokoro, T. (1997). Measurement of temporal summation of visual acuity with use of modified tachistoscope. Japanese Journal of Ophthalmology, 41(6), 403-408. doi:DOI: 10.1016/S0021-5155(97)00082-8
Norton, J. W., & Corbett, J. J. (2000). Visual perceptual abnormalities: hallucinations and illusions Seminars in Neurology, 20(1), 111-121.
Visual perceptual abnormalities may be caused by diverse etiologies which span the fields of psychiatry and neurology. This article reviews the differential diagnosis of visual perceptual abnormalities from both a neurological and a psychiatric perspective. Psychiatric etiologies include mania, depression, substance dependence, and schizophrenia. Common neurological causes include migraine, epilepsy, delirium, dementia, tumor, and stroke. The phenomena of palinopsia, oscillopsia, dysmetropsia, and polyopia among others are also reviewed. A systematic approach to the many causes of illusions and hallucinations may help to achieve an accurate diagnosis, and a more focused evaluation and treatment plan for patients who develop visual perceptual abnormalities. This article provides the practicing neurologist with a practical understanding and approach to patients with these clinical symptoms.Nousiainen, I., Kälviäinen, R., & Mäntyjärvi, M. (2000). Color vision in epilepsy patients treated with vigabatrin or carbamazepine monotherapy. Ophthalmology, 107(5), 884-888. doi:DOI: 10.1016/S0161-6420(00)00077-4
PurposeO'Shea, B., & Fagan, J. (2001). Lysergic acid diethylamide. Irish Medical Journal, 94(7), 217.
Osmond, H. (1973). The medical and scientific importance of hallucinogens. The Practitioner, 210(255), 112-119.
Palenzona, C. (1968). Hallucinogens. Medical and social aspects. [Gli allucinogeni. Gli aspetti medici e sociali] Minerva Medica, 59(46 Suppl), 15-17.
Passie, T., Schneider, U., & Emrich, H. M. (2002). Persisting continuous visual perception disorder in a chronic MDMA ('ecstasy') user. The Australian and New Zealand Journal of Psychiatry, 36(2), 266-267.
Paulsen, H. G., & Laeng, B. (2006). Pupillometry of Grapheme-Color Synaesthesia. Cortex, 42(2), 290-294. doi:DOI: 10.1016/S0010-9452(08)70354-X
Perel, A., & Davidson, J. T. (1976). Recurrent hallucinations following ketamine. Anaesthesia, 31(8), 1081-1083.
Recurrent hallucinations appeared in an 11-year-old boy during 5 days following ketamine anaesthesia. Previous anaesthesia with ketamine and adequate diazepam supplementation did not produce any such effect. The phenomenon of delayed recurring hallucinations is a rare but dangerous side-effect of ketamine, not unlike LSD flashbacks. The described case lends support to previous reports on the value of diazepam in the prevention of post-ketamine perceptual abnormalities.Rickert, V. I., Siqueira, L. M., Dale, T., & Wiemann, C. M. (2003). Prevalence and risk factors for LSD use among young women. Journal of Pediatric and Adolescent Gynecology, 16(2), 67-75.
STUDY OBJECTIVE: To report the lifetime prevalence of lysergic acid diethylamide (LSD) and to identify unique correlates of using this substance in the last year among a large multiethnic sample of sexually active adolescent and young adult women aged 14 to 26 yrs. DESIGN, SETTING, PARTICIPANTS: A cross-sectional survey, administered at university-based ambulatory reproductive health clinics, was completed by 904 women between April and November of 1997 to identify risk factors associated with their use of LSD within the past 12 months. Subjects who reported lifetime, but not past 12 months', use of marijuana, LSD, or other illicit drugs were excluded, leaving a sample of 368 nonusers and 56 users of LSD. In addition, 231 young women who reported only using marijuana in the last year were used as a comparison group to identify unique factors associated with LSD use. RESULTS: Of the total sample (n=904), 13% (n=119) reported lifetime use of LSD, and 58% (n=536) reported lifetime use of marijuana. Logistic regression analyses controlling for age and race/ethnicity found distinct profiles for those who reported using LSD or only marijuana in the last year when compared to those who reported no substance use. Common to both groups was reporting being drunk at least 10 times during the last year, regular smoking of at least half a pack of cigarettes, and identification as a high-sexual-risk taker. However, LSD users as compared to nonusers were more likely to report white ethnicity (as compared to nonwhite), be less than or equal to 17 years of age (as compared to at least 18 years), report a history of physical abuse, and be categorized as having severe depressive symptomatology. In contrast, those who reported only using marijuana were more likely to report single marital status, young age at first intercourse, having half or more of their friends use marijuana, and poor grades. CONCLUSIONS: The female LSD user presents a distinct profile that might aid clinicians in identifying potential LSD use in this population as well as alerting clinicians to the relationship between LSD use and high-risk sexual behaviors.Ryan, R. E., Prictor, M. J., McLaughlin, K. J., & Hill, S. J. (2008). Audio-visual presentation of information for informed consent for participation in clinical trials. Cochrane Database of Systematic Reviews (Online), (1)(1), CD003717. doi:10.1002/14651858.CD003717.pub2
BACKGROUND: Informed consent is a critical component of clinical research. Different methods of presenting information to potential participants of clinical trials may improve the informed consent process. Audio-visual interventions (presented for example on the Internet, DVD, or video cassette) are one such method. OBJECTIVES: To assess the effects of providing audio-visual information alone, or in conjunction with standard forms of information provision, to potential clinical trial participants in the informed consent process, in terms of their satisfaction, understanding and recall of information about the study, level of anxiety and their decision whether or not to participate. SEARCH STRATEGY: We searched: the Cochrane Consumers and Communication Review Group Specialised Register (searched 20 June 2006); the Cochrane Central Register of Controlled Trials (CENTRAL), The Cochrane Library, issue 2, 2006; MEDLINE (Ovid) (1966 to June week 1 2006); EMBASE (Ovid) (1988 to 2006 week 24); and other databases. We also searched reference lists of included studies and relevant review articles, and contacted study authors and experts. There were no language restrictions. SELECTION CRITERIA: Randomised and quasi-randomised controlled trials comparing audio-visual information alone, or in conjunction with standard forms of information provision (such as written or oral information as usually employed in the particular service setting), with standard forms of information provision alone, in the informed consent process for clinical trials. Trials involved individuals or their guardians asked to participate in a real (not hypothetical) clinical study. DATA COLLECTION AND ANALYSIS: Two authors independently assessed studies for inclusion and extracted data. Due to heterogeneity no meta-analysis was possible; we present the findings in a narrative review. MAIN RESULTS: We included 4 trials involving data from 511 people. Studies were set in the USA and Canada. Three were randomised controlled trials (RCTs) and the fourth a quasi-randomised trial. Their quality was mixed and results should be interpreted with caution.Considerable uncertainty remains about the effects of audio-visual interventions, compared with standard forms of information provision (such as written or oral information normally used in the particular setting), for use in the process of obtaining informed consent for clinical trials. Audio-visual interventions did not consistently increase participants' levels of knowledge/understanding (assessed in four studies), although one study showed better retention of knowledge amongst intervention recipients. An audio-visual intervention may transiently increase people's willingness to participate in trials (one study), but this was not sustained at two to four weeks post-intervention. Perceived worth of the trial did not appear to be influenced by an audio-visual intervention (one study), but another study suggested that the quality of information disclosed may be enhanced by an audio-visual intervention. Many relevant outcomes including harms were not measured. The heterogeneity in results may reflect the differences in intervention design, content and delivery, the populations studied and the diverse methods of outcome assessment in included studies. AUTHORS' CONCLUSIONS: The value of audio-visual interventions for people considering participating in clinical trials remains unclear. Evidence is mixed as to whether audio-visual interventions enhance people's knowledge of the trial they are considering entering, and/or the health condition the trial is designed to address; one study showed improved retention of knowledge amongst intervention recipients. The intervention may also have small positive effects on the quality of information disclosed, and may increase willingness to participate in the short-term; however the evidence is weak. There were no data for several primary outcomes, including harms. In the absence of clear results, triallists should continue to explore innovative methods of providing information to potential trial participants.Further research should take the form of high-quality randomised controlled trials, with clear reporting of methods. Studies should conduct content assessment of audio-visual and other innovative interventions for people of differing levels of understanding and education; also for different age and cultural groups. Researchers should assess systematically the effects of different intervention components and delivery characteristics, and should involve consumers in intervention development. Studies should assess additional outcomes relevant to individuals' decisional capacity, using validated tools, including satisfaction; anxiety; and adherence to the subsequent trial protocol.Saidel, D. R., & Babineau, R. (1976). Prolonged LSD flashbacks as conversion reactions. The Journal of Nervous and Mental Disease, 163(5), 352-355.
This paper presents a case study of the background and treatment of a patient with prolonged LSD flashbacks. The hypothesis that flashbacks can be psychologically determined symptoms is supported by the dynamics of the case and the course of treatment. A second focus is a partial explanation for the often made observation that obessive-compulsive personalities are at increased risk for LSD flashbacks.Scott, M. E. (1971). The flashback phenomenon. Virginia Medical Monthly, 98(6), 317-320.
Seal, R. E. (1970). The current status of the hallucinogenic drugs. The Australian and New Zealand Journal of Psychiatry, 4(1), 64-67.
Sierras-Siegart, M. (2008). Despersonalization: Clinical and Neurobiological Aspects. Colombia Psiquiatry Review, 37(1), 40-55.
Simeon, D., Kozin, D. S., Segal, K., & Lerch, B. (2009). Is depersonalization disorder initiated by illicit drug use any different? a survey of 394 adults. The Journal of Clinical Psychiatry, doi:10.4088/JCP.08m04370
OBJECTIVE: Previous studies have documented that in a substantial minority of individuals with depersonalization disorder, onset is first triggered by illicit drug ingestion. The goal of this study was to systematically compare a large sample of individuals with drug-initiated (D) versus non-drug-initiated (ND) chronic depersonalization. METHOD: We conducted an internet survey of 394 adults endorsing DSM-IV-TR depersonalization and/or derealization symptoms. Sixty-four questions were utilized to inquire about demographic and clinical characteristics, illness course, substance use history, and treatment response. The Cambridge Depersonalization Scale (CDS) was administered. The study was conducted from September 2005 to January 2006. RESULTS: Compared to the ND group (n = 198), the D group (n = 196) included more male and younger individuals. The 2 most common precipitating drugs were cannabis and hallucinogens, followed by ecstasy. The majority of participants had modest use histories prior to onset and never ingested subsequently. The 2 groups endorsed similar illness course, impairment, suicidality, and limited treatment response. The D group showed significantly greater improvement over time than the ND group (P = .002), although the groups did not differ in reported psychotherapy or pharmacotherapy effectiveness. The groups did not differ in CDS total score or on the 4 subscale scores of unreality of self, perceptual alterations, unreality of surroundings, and temporal disintegration. On the numbing subscale of the CDS, the ND group scored higher (P = .009) only prior to controlling for age and gender. CONCLUSION: The study strongly supports a uniform syndrome for chronic depersonalization/derealization regardless of precipitant.Simeon, D., Kozin, D. S., Segal, K., Lerch, B., Dujour, R., & Giesbrecht, T. (2008). De-constructing depersonalization: further evidence for symptom clusters. Psychiatry Research, 157(1-3), 303-306. doi:10.1016/j.psychres.2007.07.007
Depersonalization disorder is defined in the DSM-IV-TR using a single symptom criterion, which does not do justice to the phenomenological complexity of the disorder. In 394 affected adults, the Cambridge Depersonalization Scale yielded five factors (numbing, unreality of self, perceptual alterations, unreality of surroundings, and temporal disintegration), put forth as symptom criteria for a better diagnosis of depersonalization disorder.Smith, J. A., Walters, G., & Johnston, D. (1980). LSD 'flashback' as a cause of diagnostic error. Postgraduate Medical Journal, 56(656), 421-422.
An emaciated, but otherwise physically normal young man presented with an acute psychosis resembling hallucinogenic drug abuse. His behaviour was so strange that the underlying pathology of severe pyloric stenosis was only detected when a chance measurement of urea and electrolytes was made, revealing gross biochemical abnormalities. His abnormal mental state persisted for more than one week and an LSD 'flashback' was postulated as the cause of the prolonged psychosisStein, D. J., & Simeon, D. (2009). Cognitive-affective neuroscience of depersonalization. CNS Spectrums, 14(9), 467-471.
Depersonalization disorder (DPD) is characterized by a subjective sense of detachment from one's own being and a sense of unreality. An examination of the psychobiology of depersonalization symptoms may be useful in understanding the cognitive-affective neuroscience of embodiment. DPD may be mediated by neurocircuitry and neurotransmitters involved in the integration of sensory processing and of the body schema, and in the mediation of emotional experience and the identification of feelings. For example, DPD has been found to involve autonomic blunting, deactivation of sub-cortical structures, and disturbances in molecular systems in such circuitry. An evolutionary perspective suggests that attenuation of emotional responses, mediated by deactivation of limbic structures, may sometimes be advantageous in response to inescapable stress.Stone, A. L., O'Brien, M. S., De La Torre, A., & Anthony, J. C. (2007). Who is becoming hallucinogen dependent soon after hallucinogen use starts? Drug and Alcohol Dependence, 87(2-3), 153-163. doi:10.1016/j.drugalcdep.2006.08.008
This study, based upon epidemiological survey data from the United States (U.S.) National Household Surveys on Drug Abuse (NHSDA) from 2000 to 2001, presents new estimates for the risk of developing a hallucinogen dependence syndrome within 24 months after first use of any hallucinogen (median elapsed time approximately 12 months). Subgroup variations in risk of becoming hallucinogen dependent also are explored. Estimates are derived from the NHSDA representative samples of non-institutionalized U.S. residents ages 12 and older (n=114,241). A total of 2035 respondents had used hallucinogens for the first time within 24 months prior to assessment. An estimated 2-3% of these recent-onset hallucinogen users had become dependent on hallucinogens, according to the NHSDA DSM-IV computerized diagnostic algorithm. Controlling for sociodemographic and other drug use covariates, very early first use of hallucinogens (age 10-11 years) is associated with increased risk of hallucinogen dependence (p<0.01). Excess risk of developing hallucinogen dependence was found in association with recent-onset use of mescaline; excess risk also was found for recent-onset users of ecstasy and of PCP. This study's evidence is consistent with prior evidence on a tangible but quite infrequent dependence syndrome soon after the start of hallucinogen use; it offers leads that can be confirmed or disconfirmed in future investigations.Stone, A. L., Storr, C. L., & Anthony, J. C. (2006). Evidence for a hallucinogen dependence syndrome developing soon after onset of hallucinogen use during adolescence. International Journal of Methods in Psychiatric Research, 15(3), 116-130.
This study uses latent class methods and multiple regression to shed light on hypothesized hallucinogen dependence syndromes experienced by young people who have recently initiated hallucinogen use. It explores possible variation in risk. The study sample, identified within public-use data files of the 1999 National Household Survey on Drug Abuse (NHSDA), consists of 1186 recent-onset hallucinogen users, defined as having initiated hallucinogen use within 24 months of assessment (median elapsed time since onset of use -12 to 13 months). The recent-onset users in this sample were age 12 to 21 at the time of assessment and were between the ages of 10 and 21 at the time of their first hallucinogen use. The NHSDA included items to assess seven clinical features often associated with hallucinogen dependence, which were used in latent class modelling. Latent class analysis, in conjunction with prior theory, supports a three-class solution, with 2% of recent-onset users in a class that resembles a hallucinogen dependence syndrome, whereas 88% expressed few or no clinical features of dependence. The remaining 10% may reflect users who are at risk for dependence or in an early stage of dependence. Results from latent class regressions indicate that susceptibility to rapid transition from first hallucinogen use to onset of this hallucinogen dependence syndrome might be influenced by hallucinogenic compounds taken (for example, estimated relative risk, RR = 2.4, 95% CI = 1.6, 7.6 for users of MDMA versus users of LSD). Excess risk of rapid transition did not appear to depend upon age, sex, or race/ethnicity.Strassman, R. J. (1984). Adverse reactions to psychedelic drugs. A review of the literature. The Journal of Nervous and Mental Disease, 172(10), 577-595.
The use of naturally occurring and synthetically derived compounds for their "psychedelic" effects has been a part of human culture for thousands of years. The basic pharmacology of the major synthetic psychedelic compounds (primarily lysergic acid diethylamide [LSD]-25) is described and reference is made to their potentially beneficial psychological effects. Adverse reactions, defined as dysphoric and/or maladaptive/dysfunctional responses to the use of these drugs, sometimes require careful clinical judgment in order to diagnose. These reactions can be effectively classified along a temporal continuum. Acute, short-lived reactions are often fairly benign, whereas chronic, unremitting courses carry a poor prognosis. Delayed, intermittent phenomena ("flashbacks") and LSD-precipitated functional disorders that usually respond to treatment appropriate for the non-psychedelic-precipitated illnesses they resemble, round out this temporal means of classification. The question of organic brain damage as well as permanent changes in personality, attitudes, and creativity in patients and normals who have repeatedly ingested psychedelic drugs is controversial, but tends to point to subtle or nonsignificant changes. Future areas for study of the psychedelics' pharmacological, psychological, and therapeutic effects are suggested.Strassman, R. J. (1995). Hallucinogenic drugs in psychiatric research and treatment. Perspectives and prospects. The Journal of Nervous and Mental Disease, 183(3), 127-138.
Clinical research with hallucinogens has resumed after a generation's hiatus. To place these new studies in context, this article reviews the history of hallucinogens' use and abuse, discusses their pharmacological properties, and highlights previous human studies. Research with lysergic acid diethylamide and related hallucinogens with thousands of patients and control subjects was associated with acceptable safety when subjects were carefully screened, supervised, and followed up. Data were generated regarding hallucinogens' psychopharmacology, overlap with endogenous psychoses, and psychotherapeutic efficacy. Current American and European studies emphasize systematic psychopharmacology, in addition to psychotherapy protocols. Human hallucinogen research will help define unique mind-brain interfaces, and provide mechanistic hypotheses and treatment options for psychiatric disorders. It is critical that human hallucinogen research in the 1990s make use of state of the art methodologies, or consensually define when modifications are required. Training and supervisory issues also must be explicitly addressed.Sunness, J. S. (2004). Persistent afterimages (palinopsia) and photophobia in a patient with a history of LSD use. Retina (Philadelphia, Pa.), 24(5), 805.
Taffe, M. A., Weed, M. R., Davis, S., Huitron-Resendiz, S., Schroeder, R., Parsons, L. H., Henriksen, S. J., & Gold, L. H. (2001). Functional consequences of repeated (+/-)3,4-methylenedioxymethamphetamine (MDMA) treatment in rhesus monkeys. Neuropsychopharmacology : Official Publication of the American College of Neuropsychopharmacology, 24(3), 230-239. doi:10.1016/S0893-133X(00)00185-8
Six rhesus monkeys were trained to stable performance on neuropsychological tests of memory, reinforcer efficacy, reaction time and bimanual motor coordination. Three monkeys were then exposed to a high-dose, short course regimen of (+/-)3,4-Methylenedioxymethamphetamine (MDMA, "Ecstasy") (4 days, 10 mg/kg i.m., b.i.d.). Following treatment, concentrations of 5-hydroxyindoleacetic acid (5-HIAA) in cerebrospinal fluid (CSF) were reduced by approximately 50% in the treated animals, and this effect persisted for approximately three months post-MDMA. Behavioral performance was disrupted during acute MDMA treatment but returned to baseline within one week following treatment. MDMA also produced persistent alterations in late peak latencies of brainstem auditory evoked potentials (BSAEP), lasting three months post-MDMA. Both CSF 5-HIAA concentrations and evoked potential latencies were normalized four months after treatment. These findings indicate that serotonergic alterations associated with MDMA use may result in persisting changes in brain function.Teeple, R. C., Caplan, J. P., & Stern, T. A. (2009). Visual hallucinations: differential diagnosis and treatment Primary Care Companion to the Journal of Clinical Psychiatry, 11(1), 26-32.
Vecellio, M., Schopper, C., & Modestin, J. (2003). Neuropsychiatric consequences (atypical psychosis and complex-partial seizures) of ecstasy use: possible evidence for toxicity-vulnerability predictors and implications for preventative and clinical care. Journal of Psychopharmacology (Oxford, England), 17(3), 342-345.
Two case reports of ecstasy abuse and its serious neuropsychiatric complications are presented. The first patient developed a florid paranoid psychosis resembling schizophrenia after repeated long-term recreational ecstasy abuse, and significant alterations with intermittent paroxysmal discharges were found in his electroencephalogram. The second patient showed an atypical paranoid psychosis with Fregoli syndrome and a series of complex-partial epileptic seizures with secondary generalization after a first single ecstasy dose. Both subjects presented considerable vulnerability; the first a minimal brain dysfunction after perinatal asphyxia and a persisting attention deficit/hyperactivity disorder, the second a long-lasting opioid addiction. In vulnerable individuals, dose-independent ecstasy abuse can lead to unpredictable and potentially dangerous neuropsychiatric sequelae which require proper initial assessment and adequate treatment.Weber, P., Ruof, H., & Jourdan, S. (2005). Differential diagnosis of visual hallucinations [Differenzialdiagnose visueller Trugbilder ] Klinische Padiatrie, 217(1), 25-30. doi:10.1055/s-2004-818792
OBJECTIVE: Visual hallucinations in children need a differential diagnostic effort. METHODS AND PATIENTS: In a retrospective cohort study we identified all children, admitted to the Department of Neuropediatrics of a University Hospital between 1.1.2001 and 31.12.2003 suffering from visual hallucinations. All children underwent neurologic examination and electroencephalography (EEG). RESULTS: 14 children with visual hallucinations were identified. Disturbed perception of the size (9 of 14 cases), of the form (5 of 14 cases), and irregular perceptions of movements (5 of 14 cases) were most frequently reported. One child showed a transient hemihypesthesia, the only pathologic finding in the neurologic examination. Three children had features of hypersynchronic activity in EEG: one child undergoing immunosuppressive drug therapy and with a visual hallucination in context of a reversible posterior leucoencephalopathy showed a focal slow background activity, whereas three children had a sharp wave activity. Two of these children fulfilled the criteria for a focal epilepsy, one of them of the frontal lobe, one of the temporal lobe. CONCLUSION: Recurrent visual hallucinations are frequently transient and show clinical and pathophysiologic features reminiscent of infantile migraine. Psychic etiology, focal epilepsy and, under special circumstances, a reversible posterior leucoencephalopathy have to be considered when making a differential diagnosis.Wesson, D. R., & Smith, D. E. (1976). An analysis of psychedelic drug flashbacks. The American Journal of Drug and Alcohol Abuse, 3(3), 425-438.
Psychedelic drug flashbacks have been a puzzling clinical phenomenon observed by clinicians. Flashbacks are defined as transient, spontaneous recurrences of the psychedelic drug effect appearing after a period of normalcy following an intoxication of psychedelics. The paper traces the evolution of the concept of flashback and gives examples of the varieties encountered. Although many drugs have been advocated for the treatment of flashback, flashbacks generally decrease in intensity and frequency with abstinence from psychedelic drugs.Wilhelm, H., & Wilhelm, B. (2003). Clinical Applications of Pupillography. Journal of Neuro-Ophthalmology, 23(1)
colon; The development of personal computer-based infrared video instruments has allowed pupillography to enter the clinical arena. Measuring pupil diameter for refractive surgery, distinguishing Horner syndrome from physiologic anisocoria, quantifying the relative afferent pupillary defect, and plotting visual fields by means of graded pupil constriction to focal light stimuli are recent applications in ophthalmology. Pupillography has also been used to determine sleepiness and autonomic effects of new pharmaceuticals. (C) 2003 Lippincott Williams & Wilkins, Inc.Woody, G. E. (1971). Hallucinogens and afterimages. The American Journal of Psychiatry, 128(3), 367.
Yager, J., Crumpton, E., & Rubenstein, R. (1983). Flashbacks among soldiers discharged as unfit who abused more than one drug. The American Journal of Psychiatry, 140(7), 857-861.
Of 280 soldiers discharged from military service in 1971 as unfit, 207 reported the heavy use of at least one drug (most of these abused more than one drug) and 146 (52%) reported having flashbacks. Most flashbacks were of a simple visual nature, but repeat "trips," complex subjective experiences, and persistent difficulties in concentration were often reported. The prevalence and severity of flashbacks increased with drug use, particularly with hallucinogens and marijuana. Because psychological, social, and physiological factors may all contribute to flashback phenomena, other populations need to be studied to determine the extent to which these findings can be generalized.Young, C. R. (1997). Sertraline treatment of hallucinogen persisting perception disorder. The Journal of Clinical Psychiatry, 58(2), 85.












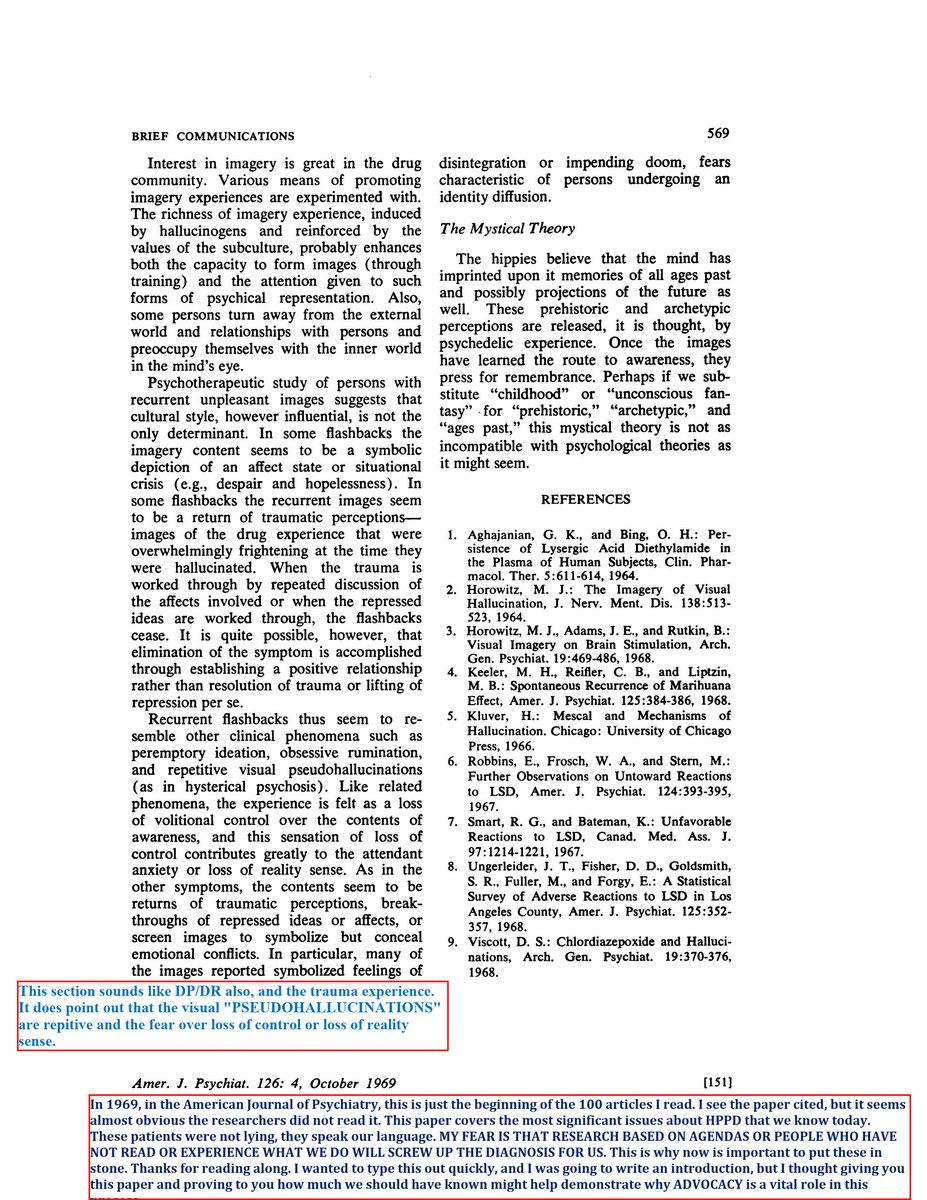












RESEARCH INTRO
in Research Articles, Publications and Studies
Posted
"Characterization, Frequency and Severity of Visual Phenomenology in Adults with Hallucinogen Persisting Perception Disorder"
Name and address of the principal investigator
David S. Kozin,
Site where the study will be performed: Online. The study will be carried out at the office of the principal investigator with 256-bit SSL encrypted server access.
Introduction
Hallucinogen Persisting Perception Disorder (HPPD) is a persisting, post-substance use disorder characterized by the diagnostic criterion of “the re-experiencing, following cessation of use of a hallucinogen, of one or more of the perceptual symptoms that were experienced while intoxicated with the hallucinogen (e.g., geometric hallucinations, false perceptions of movement in the peripheral visual fields, flashes of colors, intensified colors, trails of images of moving objects, positive afterimages, halos around objects, macropsia, and micropsia.” (DSM-5 (update definition)). Abraham (1993) completed the most complete characterization of symptoms Additionally, individuals reporting HPPD and anecdotal evidence from online support message boards suggest that a prominent portion of this population presents symptoms of depersonalization disorder and derealization without clinical memory or identity alterations typically present in other dissociative disorders (Simeon & Kozin et al, unpublished data). The course of HPPD with the most significant distress is typically chronic and continuous (Lerner et al. 2002 & online descriptions), however the DSM-5 (update definition) does not differentiate between the chronic and transient forms of perceptual disturbances as independent diagnostic entities (APA 2004).
HPPD often lasts for years and often individuals with significant symptom severity with have the disorder for over 30 years and likely will not end until the end of their lives. The triggering of the visual symptoms does not always occur immediately after the precipitant drug, but has been been reported to be associated either with trauma (self-reports) or a non-hallucinogenic drug is the precipitant, or increases symptoms (Alcántra, (1998), Favazza & Domino (1969), Lauterbach et al (2000) , Lerner et al (2002), Markel et al (1994), Morehead & Morehead (1997), Scott (1971), & Solhkhah (2000), unpublished online reports).
Dr. Roger Davis and David Kozin created a complete set of visual simulators for the symptoms described in Abraham’s 1983 symptom list. Davis and Kozin used images from individuals from an online HPPD community and completed a one week session where each visual simulator we presented to a live audience of individuals from the HPPD online community to constantly discuss with Davis and Kozin regarding the accuracy of each image. Ultimately, we need a catalogue of HPPD visual disturbances and these simulators are able to be included as tools within the survey. This could help develop an online catalogue where each "plate" in the represents a reference point through which patients can explain their vision to mental health professionals and other doctors. Unfortunately, at this point we we do not have a systematic and objective result from participants on their responses to these images. Eventually, the entire catalog of simulators could be distributed online for clinical consumption for doctors to help them understand HPPD perceptual disturbances, acquainting them with the disorder, and perhaps averting tragedies where, for example, HPPD patients are misdiagnosed with schizophrenia and given antipsychotic drugs that can worsen the disorder.
It is the goal of this survey to descriptively and systematically study in greater depth the frequency, duration, and severity of the visual symptoms of HPPD, the relationship between illicit and non-illicit drug use and HPPD-like symptoms, investigate other additional possible psychopathologies with valid instruments and/or self-report, and to investigate the differences between chronic and transient subtypes.
In light of the DSM-V’s goal of a dimensional approach to diagnosis, and also to not make the mistake of the DSM-III and IV to sacrifice validity over stability (personal communications with APA Task Force members during the ISSTD conference), a study that helps identify and improve diagnostic precision for these persisting drug-induced experiences, either transient or chronic, will help with choosing treatments and improving and clarifying research with improved definitions to match the variability in these disorders. This will improve the validity of the diagnosis, and lead to proper treatments associated with each subtype.
Mood, anxiety and personality disorders are often comorbid with HPPD, but none have been examined to predict symptom severity. The most common proximal precipitants of the disorder are hallucinogens (specifically HPPD), however non-hallucinogens have been reported to cause similar symptoms. These will be investigated by allowing non-hallucinogen users to participate if they match the visual symptom criteria and including a standard scale to measure mood and anxiety. Axis II disorders will unlikely be able to be examined within the time-frame anticipated for this study.
Reports from online forums for people with HPPD (such as the forum at http://www.hppdonline.com) and clinical experience suggests that: 1) The current DSM-5 (update definition) diagnosis for HPPD encompassed two disorders that have distinctly different etiologies and treatment responses, the clinical community lacks awareness of the complexity of this disorder (indicated by textbooks often referring only to the transient “flashback” type [examples are available]), and researchers reporting HPPD case studies often fail to mention chronic HPPD, and although treatments listed in the literature may be successful for flashback type, they are not proven to be successful in the chronic type – this could lead to unnecessary medication treatments for individuals with HPPD and increased cost of their health care. Potential subjects for this study, unsolicited and written in a public forum, often report on the message board or personal communication that the DSM-5 (update definition)’s inclusiveness of the phrase “flashbacks” in the name of the diagnosis as well as the often mis-use of the word in the literature has resulted in the clinician treating a chronic HPPD patient as one with temporary flashbacks resulting in the patient leaving therapy and not returning and feeling discouraged.
Research Objectives and Hypothesis
The purpose of this study is to investigate if the current definition of Hallucinogen Persisting Perception Disorder, excluding the criterion of the DSM-5 (update definition) requiring hallucinogen use, to produce multiple groups and to characterize the symptoms, comorbid disorders, and serve as the largest systematic study of HPPD participants to date. The study will gather accounts of people with vision problems not caused from hallucinogens and to investigate visual symptoms from drugs that have been reported in the literature. The hypothesis is that the current diagnosis truly encompasses two distinct sub types, and dimensional scales measuring the frequency, severity, and treatment responses will create two clusters within the current diagnosis.
Study Design and Research Methods
This survey will be posted on the internet, and we expect to recruit 200 participants over a 6-month period. Only individuals over the age of 18 will be eligible to take part. To expedite IRB review, one method would be to make the survey anonymous and protect the privacy of the participants by not inquiring about any identifying demographics, such as name, date of birth, address, or phone numbers, nor submission of e-mail addresses. However, including an initial phone interview, which could be done without recording personal data, could be set-up with the current survey software to have an initial interview over the phone and providing a unique “token” to an individual to ensure non-repeaters and help increase the potential that the participants do fit within our qualifications of having visual symptoms to those defined in HPPD. In this latter format, a participant will be able to take part in the study by contacting the laboratory by phone or e-mail, and afterwards the participant receive a token which will be activated after one day. When the 24 hours from the receipt of the token have elapsed, participants will be able to enter the survey page, enter their token information, and begin the survey. Upon completion of the survey, each token will no longer be useable and the participants will be debriefed.
Subjects will be recruited through HPPD related websites , other Internet forums related to drug-use, potentially advertised, and will require the participant to complete an online consent form.
Subjects will submit an online consent statement and questionnaire with questions on
1. Demographic information
2. A list of questions structured to diagnose HPPD based on DSM-5 (update definition) criteria
3. Drug History, past and current.
4. Using dimensional scales to rate frequency, duration, and severity of visual symptoms. questions will inquire about the disorder in-depth based on the information collected both in the literature and also using language collected from the community from the on-line support message board (Symptoms Descriptions and Stories from public forum are listed below).
6. Effects of treatments with self-reported measures of their effectiveness using the standard 7-point ical Global Impression – Improvement Scale (CGI-I)
8. The Sheehan Disability Scale will be administered. If the participant answers questions consistent with the DES, then they will be branched to take the Cambridge Depersonalization Scale.
7. Allow for a free-text description of symptoms and story for clinical narratives.
8. Include vision simulators and images for judging accuracy of these items.
Regarding the survey design and my discussions with Roger Davis, in terms of the psychometrics, we would consider using the Rasch
model to derive the scales with the goal of leading to uni-dimensional scales with a good distribution of item difficulties, this will be
necessary to quantify the disorder well at every point along its severity. We don't want to end up with scales that measure the disorder only at the more severe levels. Once we reach this point, we'll have a set of scales that could potentially be used in a next step for validation to be used by the individual clinician to assess an HPPD patient and be used by a researcher who wants to further investigate the syndrome (creating a uniform HPPD diagnosis versus the current variants of language in the literature where clinicians are using the same words to imply different syndromes). I believe this would be a reasonable first step, and also would produce a publication that allows for an updated review of HPPD. I realize that the DSM-III and IV sacrificed validity for reliability. In my opinion, moving back towards empirical research, it could be useful in discussing the possibility for suggesting (aligned with Lerner's publication and what we see online and in clinical settings) the consideration of lobbying for two subtypes of HPPD: transient flashbacks and continuous/chronic. Although I realize the knowledgeable clinician should consider this diagnosis correctly, we have seen in the literature the amount of flashback case studies, undifferentiated from chronic HPPD, eventually find homes in the pages of medical web sites and textbooks that characterize HPPD solely based on HPPD of the flashback variety. I have read many stories from HPPD'rs where this has caused considerable difficulty when trying to explain to the clinician the suffering caused from full-time perceptual disturbances and needing treatment to deal with their concern for its potential permanence; this often goes invalidated by the clinician because of the word "Flashbacks" associated with HPPD in the DSM-5.
The database of responses will be stored indefinitely in a locked filing cabinet. Data extracted will be stored in an SPSS data file, MySQL db, and Excel spreadsheet file saved on computers in the locked office of the principal investigator (same location).
Women and minorities will be included. Based on registration, members of online support message boards for HPPD are more often males, so we anticipate considerably greater participation among males (HPPDonline.com statistics). Subjects will not be audio- or videotaped. Subjects will not receive any payment for participation.
There are no potential risks to the subjects from participation in this study except for potential loss of confidentiality regarding their medical condition, which we minimize by keeping medical records in a locked filing cabinet in a locked office in a locked building. There are no direct benefits to the individual subject, nor is compensation provided for participation; however, the subject and society may benefit indirectly if this study leads to greater understanding of HPPD.
Descriptive statistics, two-sample comparisons between transient and chronic cases, and an exploratory factor analysis will be used to evaluate data collated from the survey. Dr. Roger Davis has agreed to help with question and study design and pilot testing the study with students in his graduate-level class on “Methodology of Psychometric Instrument Design”.
Anticipated Results and Potential Pitfalls
We expect the results will yield two psychometrically valid, clinically meaningful, and possibly conceptually discrete underlying dimensions of Hallucinogen Persisting Perception Disorder. Therefore, the derived frequency and symptom sets are well suited for a prospective field trial study using an adapted structured interview in an effort to derive clinically useful diagnostic criteria for HPPD for the DSM-V. We may also find evidence of positive and negative treatment self-reports dependent on subtype (for instance, greater efficacy of clonazepam for symptom reduction in chronic sub-type over periodic.) Pitfalls include that the survey precludes face-to-face diagnostics for Axis I disorders and is retrospective in nature,; however, methodological shortcomings are well recognized and characteristic of Internet-based surveys with self-referral. However, selection bias is minimized by including and advertising on targeted web sites to include individuals reporting to fit in the diagnosis and including questions designed to target individuals likely to be exaggerating symptoms, and possible inclusion of other validated scales. Additionally, using the initial phone inclusion method could help reduce common problems with online surveys. A prior online survey yielded strikingly similar results on standardized scales compared to those including diagnositics (Simeon & Kozin et al 2008 & Simeon & Kozin et al 2009)
Discussion of Next Steps
If acute and chronic types do form two distinct quantitatively valid subtypes, then two-sample comparisons between both groups and also between the hallucinogen-induced and non-hallucinogen induced groups will help will provide evidence for the difference between these groups and lead to an improved diagnosis that will follow in the spirit of the new DSM-V of designing diagnoses with the goal of ultimately benefiting the patient and lead to improved clarity of diagnosis for improved research. The study would score severity and frequency and seek a possible dimensional model for symptom descriptions, uncovering an effective HPPD symptom lexicon that should be shared with neurologists, ophthalmologists, and mental health professionals. Defining the perceptual disturbances with unified symptom descriptions within the disorder will improve the precision of the diagnosis and lead to improved treatment methods.